DAP notes

DAP notes are one type of clinical note that counselors need to write and review and professionals in almost every therapeutic field have to keep progress notes. Many just wing it and put down whatever they want. But it can be helpful to format and organize your notes to ensure that you don’t leave anything out. DAP notes provide mental health professionals with a guide for arranging pertinent information from psychotherapy sessions. Here is a DAP note primer.
Summary
- DAP notes are a simple, time-saving format that stand for Data, Assessment, Plan and can help streamline progress note documentation that can be easily modified. Download my DAP note template for free.
- Avoiding common DAP note mistakes like overexplaining or not keeping treatment plans in focus.
- Use an EHR to save time with pre-built templates and copy note features in a secure, HIPPA compliant storage.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

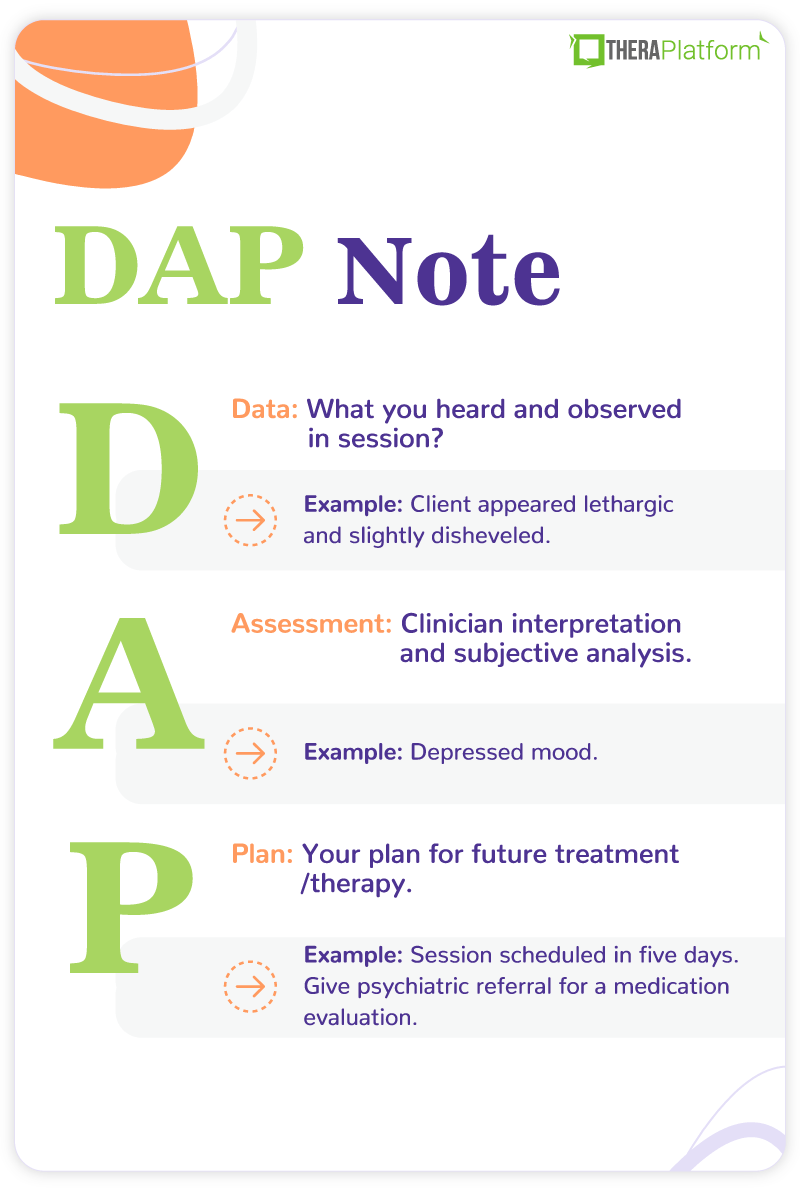
What is a DAP note?
DAP is an acronym for Data, Assessment, and Plan. It is a simple and comprehensive template to help organize your notes. It is important to recognize that a DAP note is a progress note, not a personal psychotherapy note. That means it is part of the official record and can be shared with others. Let’s explore each part of the DAP note.
DAP notes for telehealth example
→ Download My DAP Note Template for Free
DAP note components
The data component of DAP notes includes everything you heard and observed in the session. It is a review of all the information gathered. You want this section to be as objective and factual as possible. Most of this information is client self-report but clinician observations also provide valuable information. For example, they may note that a client “appears agitated”. Additionally, the data section includes interventions that the professional used in the session and the client’s response. This is similar to what you would find in a BIRP (Behavior, Intervention, Response, and Plan) note but the DAP note does not have separate sections. This is also where you would include client quotes that provide important information.
Here are some questions that are frequently answered in the data section of a DAP note:
- Why is the client here?
- How do they present themselves, including their mental status?
- Are they reporting or experiencing symptoms?
- What important events have occurred recently (since last session)?
- How have they responded to interventions from previous sessions?
- What is their behavior toward treatment? For example, are they doing their homework or missing sessions?
An overall question that summarizes this section is “what did I see and hear?”
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

DAP note assessment
The assessment portion of the DAP note reflects clinician interpretation. This is when you get to flex your clinical muscles and figure out what is going on with your client. Unlike the data section, it is primarily based upon subjective analysis.
Here are some important questions to answer in the assessment section of DAP note:
- Do you feel the client is making an effort to address their issues?
- How does the data reflect attention to their treatment goals?
- Are they making progress?
- How do they respond to interventions in session?
- Are there concerns about self-harm or harm to others?
- Does the data indicate a particular diagnosis or issue to be addressed?
- Is there any formal assessment information from testing or a screening measure?
In other words, “what does the data mean?” The assessment section is a natural follow-up to the data. Whoever is reading your note should be able to see the reasons for your assessment based on the data.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

DAP note Plan
The final portion of the DAP note is the plan for future treatment. It may involve what you want the client to do next as well as what you, the therapist, want to accomplish. For instance, you may write that the client is to complete a homework assignment or that you need to contact their psychiatrist about their medication. Keep in mind, this segment is not the entire treatment plan. It is simply the goal from one session to the next. However, it may include changes or new directions to the overall treatment plan.
Some possible questions answered in the plan section of DAP note include:
- When is the next appointment?
- Is there any homework assigned to the client?
- Any consultation needed with other professionals (e.g., a psychiatrist)?
- Any planned future interventions?
- Any changes in client goals or treatment plan?
The plan section answers the overall question, what will you do next?
What is the difference between DAP notes and SOAP notes?
If you have ever taken progress notes as an employee of a large organization, you may have been asked to use the SOAP format. The SOAP (Subjective, Objective, Assessment, and Plan) note is probably the most popular format of progress note and is used in almost all medical settings.
The main difference between SOAP and DAP notes is that the data section in a DAP note is split into subjective and objective parts. While this makes sense in a medical setting, it can be confusing when performing counseling.
This is primarily because the objective part of therapy is hard to define. Almost everything that a clinician hears is subjective. As a result, you have no way of knowing if what your client is saying to you is true.
In a medical setting, you have a lot of objective information, such as vital signs (e.g., temperature, blood pressure) and test results. The only objective information you have in a therapy session is the physical appearance of a client and maybe some psychological assessment results (and some may argue that they are objective too).
That is why many mental health professionals prefer the DAP note. You don’t have to struggle to categorize information as objective or subjective; you have the freedom to put down all the relevant information and simply include it all as “data”.
Watch this video to learn how to save time on therapy notes
DAP note tips
Make your DAP note a DARP Note:
Some people like to modify the DAP note into a DARP note, adding a place for a response after the assessment section.
This is to record the client’s response to your assessments. Some clinicians believe the response provides essential information and should, therefore, have its own section.
For example, say your client tells you they have consumed alcohol a few times this week after work. You might remark that they have been drinking a lot lately, especially after stressful days at work.
Your client might get defensive upon hearing your assessment and start making excuses. Their defensive reaction is worth noting.
In the DAP, the response is usually subsumed under the assessment piece but adding a separate section may remind you that it is important enough to consider separately. It is a matter of personal preference. Choose whatever is more effective for you.
Don’t write too much (or too little)
Remember, DAP notes are for public consumption. No one wants to read a term paper. At the same time, you need to include enough information so that someone else reading the note can understand what is happening.
One danger of the broad DAP format is that you might leave something out. Bottom line: Include essential information and get to the point.
Write your notes immediately after the session
You want your DAP note to be as accurate as possible. Unless you have an incredible memory, you are going to forget certain things that were said or done in session.
The longer you wait to document your note, the more you will forget or alter the truth. That being said, it is a good idea to write your notes as soon as possible after a session to ensure they are as accurate as possible.
Leave yourself 10 minutes between sessions so you don’t feel rushed. If you run out of time, make sure you go back to it later that same day. Never finish your day unless all your notes are completed.
Modify your DAP note
The beauty of a DAP note is that it is simple and general. It only has three sections, making it less complicated than a SOAP or BIRP note. But that doesn’t mean that you can’t divide the sections to help you organize.
In fact, the generality of the DAP note lends itself to modification to suit your needs. Don’t be afraid to add a few subsections if it helps you write the most effective note possible.
Follow the treatment plan
The treatment plan is used to guide therapy. Therefore, what you are working on in session needs to be a reflection of the treatment goals. And the DAP notes need to illustrate that you are following the treatment plan.
This is especially important in the plan section of the DAP note. Your interventions and plan for each session should be related to the goals in the treatment plan. If you find yourself focusing on an objective that isn’t included in the client’s treatment plan, that should be mentioned in your note and you will want to talk to your client about adjusting their goals.
Know your audience
Ask yourself, who is likely to read this note? Because this is not a personal psychotherapy note, it needs to be professional in tone. At the same time, your language should be easily understood by anyone who reads the note, regardless of their education level.
While you may sometimes feel like writing progress notes is inconsequential, the information in the note may be used for important purposes. The DAP note, for example, could be used to decide a client’s medication regimen or as part of a malpractice civil suit.
That means you don’t use slang terms unless you are quoting a client. As any lawyer will tell you, once it is written down, it is part of the permanent record. Proceed accordingly.
Therapy notes can be tedious, but there are ways to simplify them including centralized locations, workflow and templates.
Review your DAP notes
This sounds like common sense, but it is easy to rush through note writing and never give it a second glance.
- First, notes should be proofread for spelling and grammar. One of the strengths of writing notes online is that spelling and grammar can be easily reviewed.
- Second, is the tone professional and objective?
- Next, notes should be checked for content. Did you say everything you wanted to say or leave out anything important? Also, is what you are trying to say easily understood?
- Finally, ask yourself, would you be okay with this note if another professional saw it? How about the client?
Although you may not have time to inspect your notes right after you write them, reviewing them at the end of the day is good practice.
DAP notes examples
The following DAP note example involves someone with depressive symptoms:
Name: Jane Doe Age: 25 Date: 9/15/2022
Data: | Client appeared lethargic and slightly disheveled. Hair did not seem to be brushed and clothes were wrinkled. She reported that she had been cutting her thighs with a razor blade but denied suicidal intent or plan. She said the cutting makes her feel better. The client reported that she has been feeling a lot of financial and work stress. She would like to leave her job but feels she can’t due to the loss of income. Additionally, she is having trouble with a romantic relationship. She said that she is experiencing conflict with her mother and sister and can’t turn to them for advice. |
Assessment: | Depressed mood. She is under a lot of situational stress with limited emotional support. She also has a history of depression in her family. Denies suicidal ideation and has no history of suicidal behavior but is self-harming as a coping measure. When this therapist brought up the possibility of taking anti-depressant medication, she said she would consider it. |
Plan: | Session scheduled in five days. Give psychiatric referral for a medication evaluation. Continued assessment of self-harm and potential suicidality. Advise DBT skills to aid coping. |
The second example of a DAP note is for a client experiencing anxiety symptoms:
Name: Jane Doe Age: 40 Date: 9/25/2022
Data: | Client appeared a bit agitated. He was fidgeting and bouncing his leg. He reported difficulty sleeping because of an inability to turn off the worries in his head. He said he avoided a work happy hour because he was afraid of being judged. He also is having trouble with some of his mother’s political and cultural views but does not say anything because he doesn’t want to cause problems. He did not complete the thought record homework given last session. |
Assessment: | Client has significant anxiety in several areas of his life. His avoidance of conflict and social situations is only increasing his worries. Client does not seem highly engaged in therapy. Would rather stay in his anxious space than risk the consequences of change. Appears a bit unmotivated and stuck in his progress. |
Plan: | Session scheduled for next week. Reassigned thought record homework. Assigned daily practice of relaxation exercises. No further work will be given until the client shows more consistency with present obligations. |
Improving DAP notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized DAP (Data, Assessment, and Plan) notes.
Top 7 benefits of using EHR for DAP notes
Manually writing and storing DAP notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Automation features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the DAP note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise DAP notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
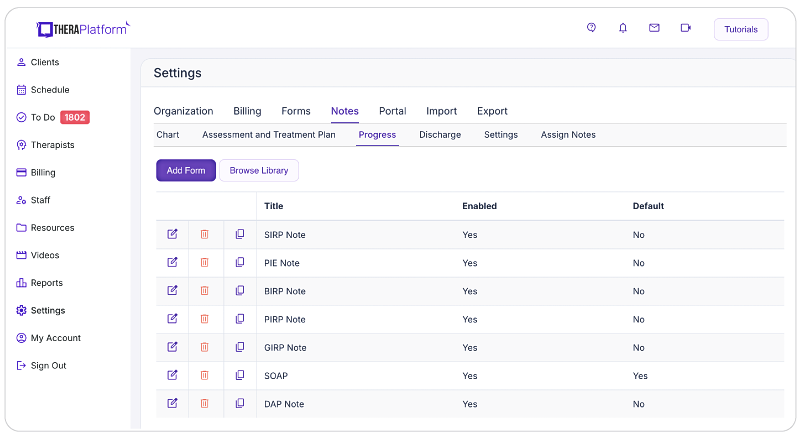
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize DAP note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating Data, Assessment, and Plan sections or using a single note field or checkboxes for mental status or techniques.

- HIPAA-compliant DAP note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard DAP notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless DAP note sharing with clients: Clients may request access to their DAP notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share DAP notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure DAP note sharing with clients.

- Duplicate DAP notes: In cases where the data remains the same across multiple sessions, duplicating DAP notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on DAP notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including DAP notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their DAP notes, allowing them more time to enhance client care.
Additional tools and outcome measures to help with data collection and progress monitoring
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners and built-in outcome measures to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as DAP notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
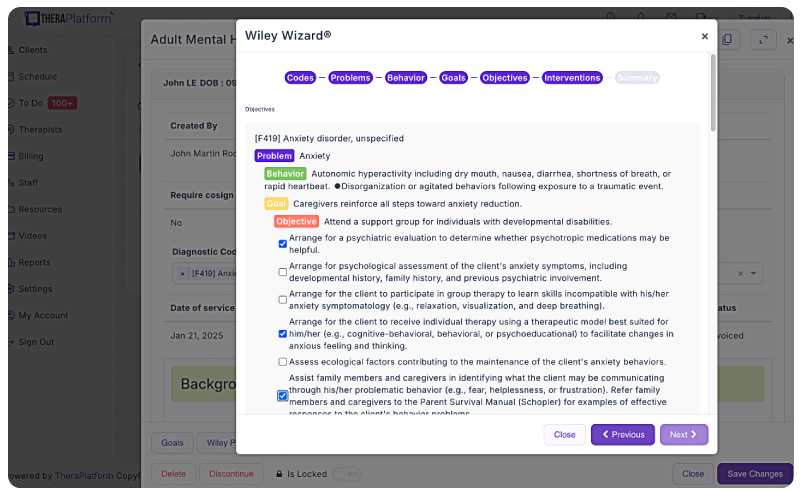
Screenshot of Wiley Treatment Planner integration into TheraPlatform illustrating how areas like problems, behaviors, goals and objectives can be completed with pre-populated, research-based statements.
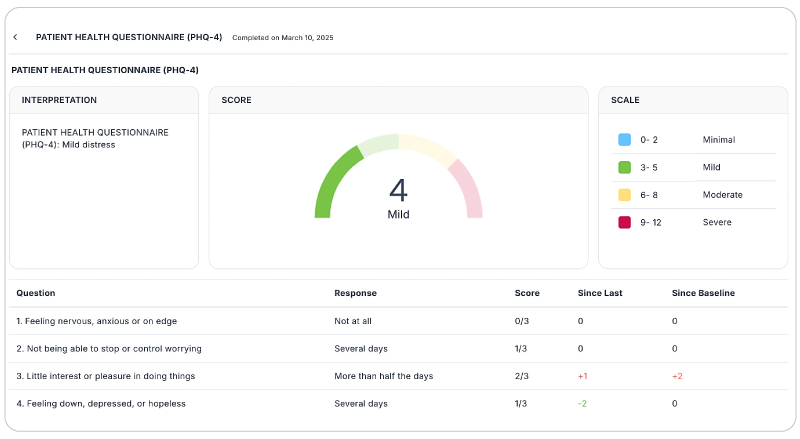
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually. However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatfrom automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Psychotherapy notes
- SOAP notes for counseling
- Crunched for time? Try concurrent documentation
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
Free video classes
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice
- Free insurance billing course for therapists
FAQs about DAP notes
What is the main purpose of a DAP note in therapy?
A DAP note organizes session details into three sections—Data, Assessment, and Plan—helping therapists document client progress clearly, support treatment planning, and maintain compliance with clinical and insurance requirements.
How do DAP notes differ from SOAP notes?
While SOAP notes divide information into Subjective, Objective, Assessment, and Plan, DAP notes simplify this process by combining subjective and objective information into one “Data” section. This makes them easier to use in counseling, where most information is subjective.
Can EHR software make writing DAP notes easier?
Yes. An EHR like TheraPlatform provides customizable templates, secure HIPPA-compliant storage, duplication features, and integrations with tools like Wiley Treatment Planner and outcome measures—streamlining note-taking and reducing administrative time.