SOAP notes counseling

A SOAP note example is used in counseling to make note-taking more consistent and accurate and save time on writing notes from scratch. See a SOAP note example, get tips for writing SOAP notes and learn how to avoid common mistakes associated with SOAP notes.
Summary
- SOAP stands for Subjective, Objective, Assessment, and Plan. This structured format helps therapists document client sessions consistently and clearly—making notes more defensible, accurate, and aligned with insurance requirements. Download my free SOAP notes template.
- Progress notes (which include counseling SOAP notes) are part of the client’s medical record and must follow HIPAA documentation standards. Psychotherapy notes, by contrast, are more detailed, stored separately, and enjoy special privacy protections under HIPAA.
- Therapists should avoid overly long narrative notes and instead focus on clarity, conciseness, and evidence-based observations. Notes should be timely, grammatically correct, and written as if they may be reviewed legally or clinically. Corrections must follow proper protocols (e.g., single strike-through with initials).
- Using an EHR like TheraPlatform allows therapists to take advantage of customizable templates, automatic scoring of outcome measures, client e-signatures, efax integration, and secure HIPAA-compliant storage. It also offers tools like the Wiley Treatment Planner for pre-written goals and interventions—saving time while supporting clinical excellence.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

What is a therapy SOAP note?
Therapy SOAP notes are the way you document that a client participated in and completed a session with you. Depending on the billing process you have, a completed therapy note may also be the way a claim is generated. Documentation also demonstrates your competency and shows how a client’s needs have been addressed.
Before talking about notes like therapy SOAP notes, know this: not all therapy notes are created equal. There are progress notes and there are psychotherapy notes.
Most therapists keep some form of therapy notes but they are very different and treated differently under HIPAA.
- Psychotherapy notes are detailed, private notes that a therapist may keep. Psychotherapy notes may contain observations, impressions and other details of the session. These notes do not follow a standard format and are stored separately. These types of notes have special protection under HIPAA and are NOT contained in the client’s record.
- Progress notes are part of the client’s record that provide details about the client such as diagnosis and assessment, symptoms, treatment and progress towards treatment goals. They follow a standard format (e.g., SOAP, BIRP, etc.) and ARE included as part of the client’s record.
Practice Management + EHR + Telehealth
Mange more in less time in your practice with TheraPlatform

.
What are the SOAP notes for mental health?
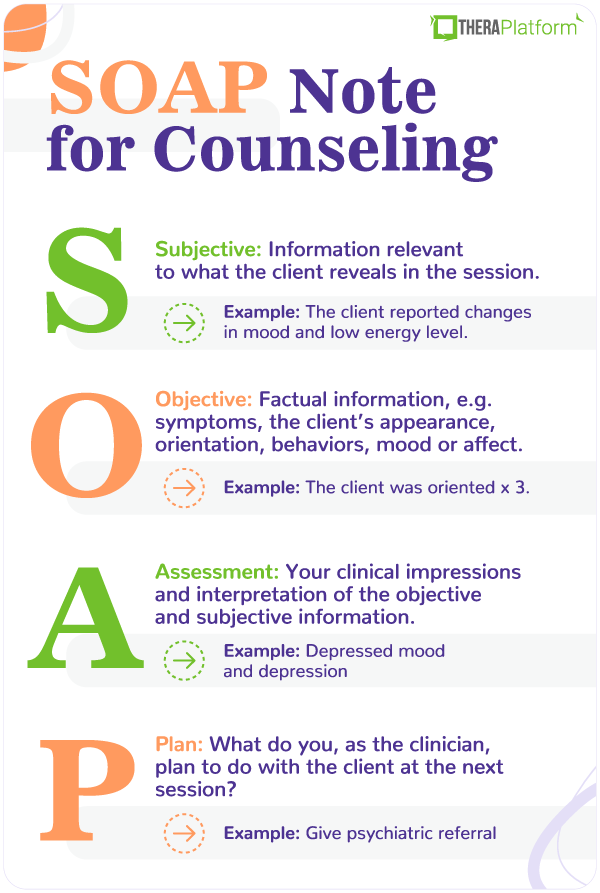
Most mental health clinicians utilize a format known as therapy SOAP notes. SOAP is an acronym that stands for:
S – Subjective
O – Objective
A – Assessment
P – Plan
Therapy SOAP notes are progress notes that contain specific information in a specific format that allows the reader to gather information about each aspect of the session.
Now, to be honest, most clinicians weren’t “trained” on therapy SOAP notes as part of graduate training. Chances are you picked up some therapy note-taking skills along the way. Some of you might be doing long, narrative notes that contain way more information than is appropriate for a progress note. (See progress vs. psychotherapy note descriptions above.)
Therapy SOAP note example
Subjective: This section contains information relevant to what the client reveals in the session. This may be the client’s chief complaint, presenting problems and any relevant information. This information may include direct quotes from the client and things discussed during the session.
- Subjective soap note example: You may have discussed your client’s complaint of not sleeping well and sleep hygiene. Use words like “Discussed” or “talked about” or “reviewed” when describing things talked about in session.
Objective: The objective section contains factual information. Such objective details may include things like a diagnosis, vital signs or symptoms, the client’s appearance, orientation, behaviors, mood or affect.
- Objective soap note example: Client is oriented x4 (person, place, time, situation), client appears disheveled.
Assessment: This section is the place where you, as the clinician, document your impressions and interpretation of the objective and subjective information. This documentation may include clinical impressions related to factors such as mood, orientation, risk of harm as well as assessment of progress towards goals. Here you want to describe your impressions.
- Assessment SOAP note example: The client appears to understand the new goal.
Plan: This section documents what the next step is for the client. What do you, as the clinician, plan to do with the client at the next session? This is also the place to document things like the anticipated frequency and duration of therapy, short and long term goals as well as any new goals. Be sure to note any homework assignments or tasks you’ve given your client.
- Plan SOAP note example: Give referral
It sounds like an easy format to follow, but it does take some practice.
Download My Free Therapy SOAP Notes Template
How do you write counseling SOAP notes for therapy?
As with any clinical documentation, you want to be sure you are including pertinent information. You also want to avoid errors that can at best be annoying and at worst, place you in legal jeopardy.
First, breathe. No therapy note is 100% perfect. Depending on who looks at it, there will always be something that could be written more clearly, more detailed, less detailed … something. The key is to write clear, thorough notes in a timely and consistent manner.
Tips for writing solid counseling SOAP notes (therapy notes):
- Write your note as if you were going to have to defend its contents.
- Use clear and concise language. Avoid using slang, poor grammar or odd abbreviations.
- Pay attention to spelling, person and tense.
- When quoting a client, be sure to place the exact words in quotation marks.
- Keep your notes short and to-the-point. Be clear and complete. Avoid expanding beyond what is required for each section.
- Be mindful of correct dates, times, spelling of names.
- Avoid making subjective statements that cannot be substantiated. When making subjective statements, include pertinent evidence. For example, client appears anxious as evidenced by wringing his hands, excessive tapping of fingers, hyperventilation.
- Never, ever alter a record using any type of correction eraser/tape/fluid/mark outs/scratch outs.
- Consider concurrent documentation and writing your therapy SOAP notes during the session.
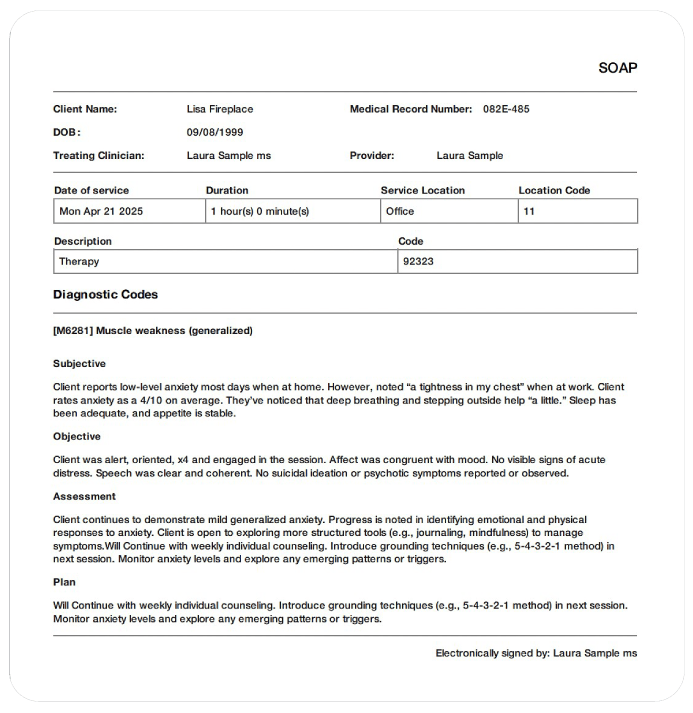
Counseling SOAP note example
Here is an example of SOAP note for counseling:
Subjective: Client reports low-level anxiety most days when at home. However, noted “a tightness in my chest” when at work. Client rates anxiety as a 4/10 on average. They’ve noticed that deep breathing and stepping outside help “a little.” Sleep has been adequate, and appetite is stable.
Objective: Client was alert, oriented, x4 and engaged in the session. Affect was congruent with mood. No visible signs of acute distress. Speech was clear and coherent. No suicidal ideation or psychotic symptoms reported or observed.
Assessment: Client continues to demonstrate mild generalized anxiety. Progress is noted in identifying emotional and physical responses to anxiety. Client is open to exploring more structured tools (e.g., journaling, mindfulness) to manage symptoms.
Plan: Will Continue with weekly individual counseling. Introduce grounding techniques (e.g., 5-4-3-2-1 method) in next session. Monitor anxiety levels and explore any emerging patterns or triggers.
Start your free trial now
How to correct a therapy SOAP notes error
Errors happen. Even the most careful note writer will make mistakes. If you find an error, resist the urge to just scratch it out or otherwise alter the record. Omissions, deletions and altered records create suspicion about its validity. The best way to correct an error is to use an accepted procedure for error correction.
Here’s an example of one such procedure:
If you find an error, use a single strike-through, write “error” next to it, and initial the error. Write in the correction and initial the correction. This way, the reader can see the original error, see the corrected information and see who made the correction. A word of caution: you want to be the one to correct your own records.
With a little practice, you can be a skilled progress note writer.
Free Resources for Therapists
Click below and help yourself to peer-created resources:
Improving SOAP notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized SOAP (Data, Assessment, and Plan) notes.
Top 7 benefits of using EHR for SOAP notes
Manually writing and storing SOAP notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Automation features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the SOAP note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise SOAP notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
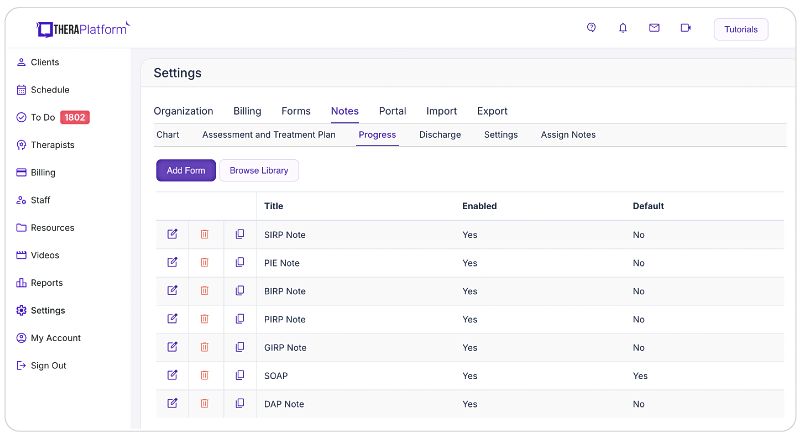
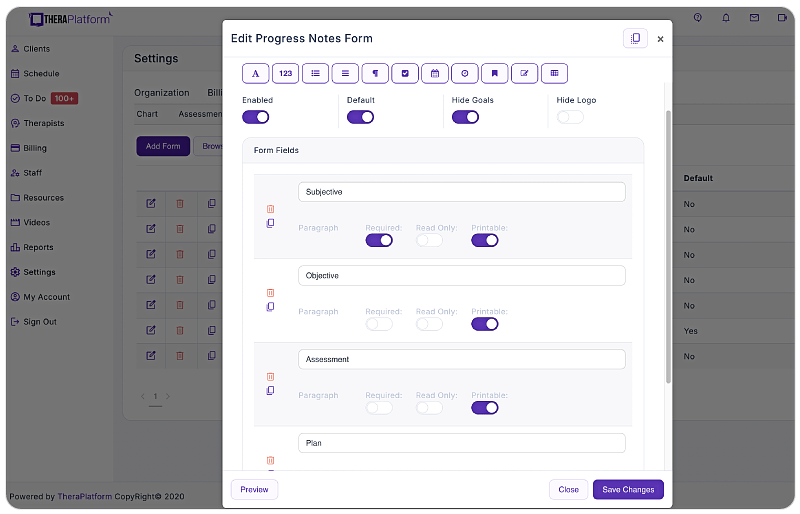
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize SOAP note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating Data, Assessment, and Plan sections or using a single note field or checkboxes for mental status or techniques.
- HIPAA-compliant SOAP note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard SOAP notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless SOAP note sharing with clients: Clients may request access to their SOAP notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share SOAP notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure SOAP note sharing with clients.
- Duplicate SOAP notes: In cases where the data remains the same across multiple sessions, duplicating SOAP notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on SOAP notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including SOAP notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their SOAP notes, allowing them more time to enhance client care.
Additional tools to help with data collection and progress monitoring for your counseling SOAP notes
Therapists and counselors can also take advantage of EHRs (such as TheraPlatfrom) that offer integrations with Wiley treatment planners for consistency on notes. The best part about partnering with a modern EHR is the time you save on formulating the documentation.
What is Wiley Treatment Planner?
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
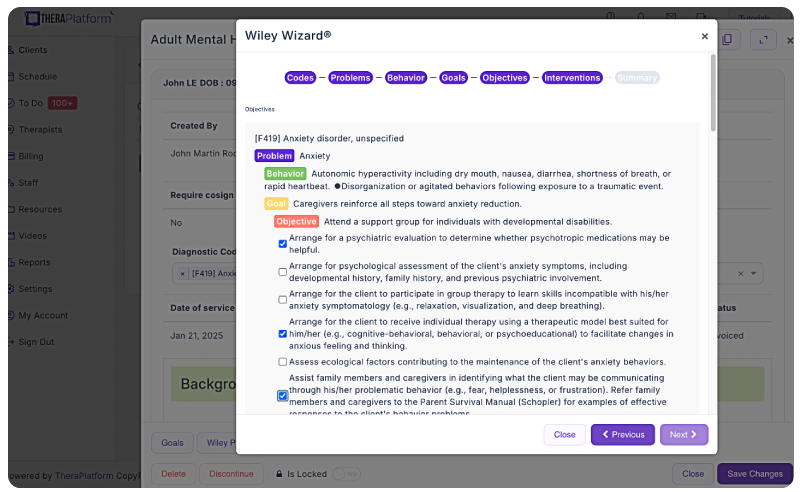
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as SOAP notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice