Psychotherapy notes

Psychotherapy notes can be as simple as scribbling down a thought during a therapy session with a client. Most clinicians keep some sort of psychotherapy notes but many professionals do not know the definition, purpose, or legal protections behind what they are writing down.
Some therapists don’t know that a psychotherapy note is not the same as a progress note. Here is everything you ever wanted to know about psychotherapy notes.
Summary
- Psychotherapy notes (or process notes) are private reflections by therapists that document or analyze the contents of a counseling session. They are separate from progress notes and excluded from the client’s official medical record. Download my free notes templates.
- Under HIPAA, psychotherapy notes are given stronger privacy protections than progress notes. They generally cannot be accessed by clients, insurers, or other providers without the therapist’s written consent, except in limited legal or safety-related situations.
- Progress notes are formal and shareable, often used for billing and clinical communication. In contrast, psychotherapy notes are for the therapist’s personal use and can be written in any format or shorthand.
- To maintain legal protections, psychotherapy notes must be stored separately from progress notes. Therapists using EHRs like TheraPlatform can safely and securely keep psychotherapy notes distinct from the clinical record.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

What is a psychotherapy note?
Psychotherapy notes—also known as process notes—have a legal definition. According to the Department of Health and Human Services, the definition of psychotherapy notes are as follows: “notes recorded (in any medium) by a health care provider who is a mental health professional documenting or analyzing the contents of conversation during a private counseling session or a group, joint, or family counseling session and that are separated from the rest of the individual's medical record.
Psychotherapy notes exclude medication prescription and monitoring, counseling session start and stop times, the modalities and frequencies of treatment furnished, results of clinical tests, and any summary of the following items: diagnosis, functional status, the treatment plan, symptoms, prognosis, and progress to date”.
Unofficially, psychotherapy notes are private notes kept by a therapist that are not meant for public consumption. They are a therapist’s thoughts, feelings, and hypotheses regarding a client. For example, you may have a theory about a client’s behavior that you aren’t quite sure is justified but might be important to consider.
Psychotherapy notes frequently include questions or concerns that might require follow-up. They do not include identifying information or formal diagnostic information. Most often, they would be taken during a session or right after a session so the therapist accurately remembers what they wanted to say while the session is fresh in his or her mind.
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

Psychotherapy notes vs progress notes
A progress note is a document of public record and can be shared with others with client consent. Although there is no absolute rule of what should be included in it, many people follow the Subjective, Objective, Assessment, and Plan (SOAP) or Data, Assessment, and Plan (DAP) note format.
Generally, as a psychotherapist, you would want to include diagnosis, symptoms, interventions, and a summary of the client’s progress.
Progress notes are designed to be easily digestible to other professionals that may read them. In contrast, psychotherapy notes are for the private use of the therapist and, therefore, can be written in any format or style the therapist desires. Indeed, some therapists quickly jot down impressions that would be unintelligible to anyone else.
Despite the technical differences between progress notes and psychotherapy notes, many therapists use them interchangeably. While hospitals and large agencies may have specific rules to follow regarding notes, therapists in smaller agencies and private practice are not subject to those rules.
They may only create one set of notes and not distinguish between psychotherapy and progress notes. This is a personal therapist decision but privacy concerns need to be considered.
HIPAA and psychotherapy notes
The Health Insurance Portability and Accountability Act (HIPAA) offers large protections for psychotherapy notes compared to progress notes. Generally, process notes cannot be shared with others if the therapist does not wish to share the information in them. On the other hand progress notes—usually with a client’s permission—are allowed to be shared with others. In some states, client consent is not even necessary. For instance, office staff may be able to access the information in a progress note without client approval.
In April 2021, the information blocking provision of the 21st Century Cures Act went into effect. In short, this law states that health care providers, including therapists, are required to share clinical notes in electronic health records (EHR) with their clients. While this applies to progress notes, psychotherapy notes are protected and not included under this provision.
It is also important to note that protections for psychotherapy notes include insurance companies. At times, insurance companies will want to audit your records to see if they want to pay for—or continue to cover—mental health services for particular clients. Under HIPAA, you may be required to give them your progress notes, but you are protected from having to share your psychotherapy notes.
Despite the protections afforded to psychotherapy notes, they can still be made public under certain situations. A judge can order a therapist to turn over psychotherapy notes for a legal case or they may need to be divulged under the threat of public safety (i.e., an abusive situation or the client being a threat to themselves or others). Although it would take a more extreme case to have psychotherapy notes released against a therapist’s will, no psychotherapy note is guaranteed 100 percent privacy.
Watch this video to learn how to simplify note taking
→ Start My Free Trial
→ Start My Free Trial
Can clients access psychotherapy notes?
Generally, no. Psychotherapy notes receive the utmost protection according to the law. Not even the clients themselves can see them without your permission. That includes the parents of minor clients as well. However, a small number of state laws may provide exceptions. For example, in Vermont, clients are allowed to see their psychotherapy notes. This is because Vermont state law offers more protections to clients than is given under HIPAA. The moral of the story: know the privacy laws that apply to your place of practice.
Is there a reason to share psychotherapy notes?
We have established that the privacy of process notes is almost always protected under the law. But that does not mean you can’t show them to other people.
Here are some reasons you may want to share them with someone else:
Transferring a client to another therapist
There are various reasons that a client may wish to change therapists. Maybe they are moving out of the area or they just don’t feel like the therapist is a good fit. In any case, it is usual practice to transfer their records to the new clinician. While treatment plans and progress notes should be included, you may wonder if you should also provide psychotherapy notes. You certainly aren’t obligated to do so but they may provide a clearer overall picture of your client’s issues than progress notes alone. Of course, there are potential drawbacks: they may be misinterpreted, misunderstood, or hinder the new therapist from forming objective opinions about the client.
Coordinating care with another professional
It is not uncommon for clients to see another professional as an adjunct to their treatment. For example, seeing a psychiatrist or a nurse practitioner to prescribe psychotropic medication is a regular occurrence when someone is in therapy. While it may be most desirable to obtain consent to speak to them directly, you may also feel it is helpful for another clinician to see your progress and psychotherapy notes. The person prescribing medication, for instance, often has limited information because they usually do not meet with the client as frequently as you do. The more data you can provide them the better. Ultimately, it is more important that they prescribe the correct medication for your client than it is for you to keep your notes to yourself.
Improve treatment progress
It is understandable that therapists would be hesitant to share their psychotherapy notes with their clients. But what if it would help their treatment? In a pilot study, researchers found that participants felt more engaged in therapy as a result of seeing psychotherapy notes about their cases. Yes, a few felt offended by what they read but the large majority of respondents felt it was a good practice that made them feel more invested in their treatment. Of course, you need to be highly sensitive when writing notes if you are considering sharing them with your clients or their family members.
If you are going to release psychotherapy notes to anyone else for any reason, it is required that you get the written authorization of the client. The only exceptions are if you are reporting abuse or neglect, or if there is a significant threat to the client’s safety.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

Tips and considerations for psychotherapy notes
- Even with psychotherapy notes, which have many HIPAA protections, you want to be careful with what you put into them. As mentioned above, no note is entirely confidential. You want to feel free to take down relevant notations but watch for incriminating information. A good rule is to never put down any information you would not want a judge, a lawyer, or the police to be able to see.
- Psychotherapy notes should exclude the information you might put in a progress note. For example, you would not put prescription medications or demographic information in a process note. It is critical to avoid blurring the boundary between a progress note and a psychotherapy note. If your psychotherapy notes start looking like your progress notes, it could be argued that they should not be subject to more stringent privacy laws.
- Some therapists develop a shorthand for psychotherapy notes so they do not have to worry as much about someone else getting a hold of their contents. Just make sure you can read your own notes.
- Psychotherapy notes should always be kept separate from progress notes. If psychotherapy notes are kept with the rest of client documentation, it is not possible to keep them private; it can be argued that they are part of the official record and they will not be protected under the same laws as psychotherapy notes.
- Know the privacy laws of the states in which you practice. State laws and HIPAA statutes may differ when it comes to privacy. In those cases, whichever is more protective of client rights is usually followed. Therefore, you may believe that your psychotherapy notes are protected by HIPAA only to find out that state law supersedes federal statutes.
- The police are not entitled to your psychotherapy notes without a court order. While you may feel pressure to turn over all your records if the police request them, you can politely ask that they go to a judge to obtain a court order.
- If your psychotherapy notes are subpoenaed, that does not necessarily mean you have to hand them over.
You can take the following actions to attempt to keep them from becoming public:
- First, make sure that your psychotherapy notes are specifically being requested. If there is only a general request for a client’s records, then you are not obligated to hand over your process notes.
- Negotiate with the person requesting your notes. This is likely a lawyer. There is no rule that says you can’t contact the lawyer and negotiate with them. It may not always work but it is worth a try.
- File a motion to quash. This is a formal request you make to the court to prevent having to provide the requested information. You will state the reasons you feel the information should not be shared.
- File a protective order. This is somewhat of a compromise. You agree that you will provide the requested information but you want to define who is allowed access to it. It is an attempt to limit any negative consequences of having the information disclosed.
- Make sure the request for records is from a judge. In certain states, a lawyer can write their own subpoena that might not hold up when challenged.
Psychotherapy notes are an integral part of treatment that are protected under stringent privacy laws. For that reason, you want to make sure to keep them separate from a client’s progress notes and the rest of their medical record.
Improving notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.
- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.
- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
Additional tools to help with data collection and progress monitoring
Therapists can also take advantage of EHRs (such as TheraPlatfrom) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
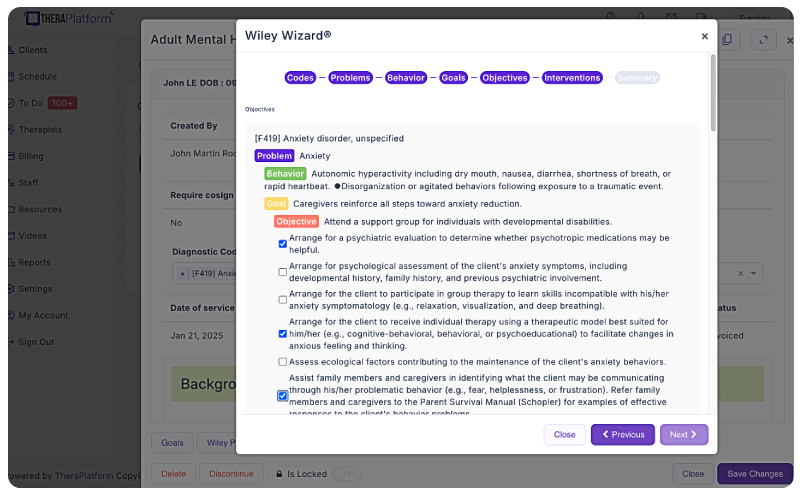
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- SOAP notes
- SOAP notes worksheets
- Wiley treatment planners
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice