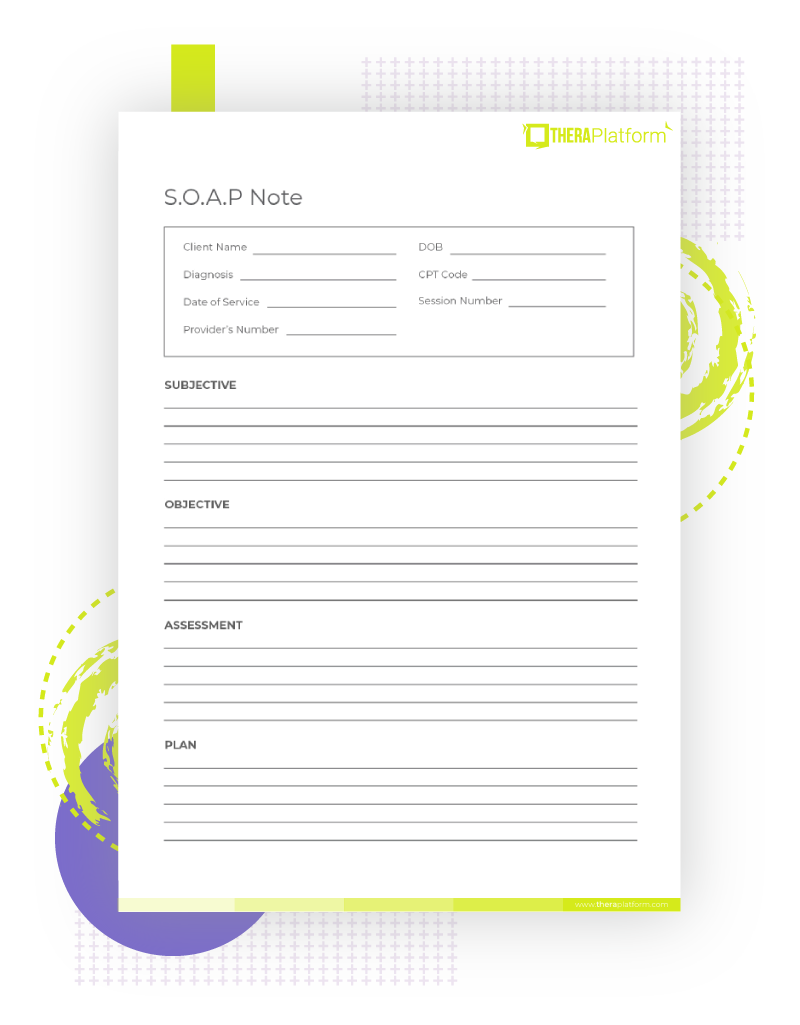
SOAP Notes Template
SOAP notes provide details from client visits and lets you communicate important information to other healthcare providers. This is a standardized form of note-taking that be used to reliably share information to other health professionals. Download our free SOAP Notes PDF template.

