Therapeutic interventions and documentation

Therapeutic interventions are the core of treatment and mental health professionals know success lies in the interventions chosen and how well they're documented.
Summary
- Therapeutic interventions must be documented with precision to ensure ethical treatment, continuity of care, and support for insurance reimbursement. Using formats like SOAP, DAP, or BIRP helps standardize note-taking and enhances clarity for future reference or clinical collaboration. Download free note templates.
- Vague statements like “discussed anxiety” are insufficient. Strong documentation specifies the intervention (e.g., CBT thought log, EMDR reprocessing), the clinical rationale, and observable or reported client responses.
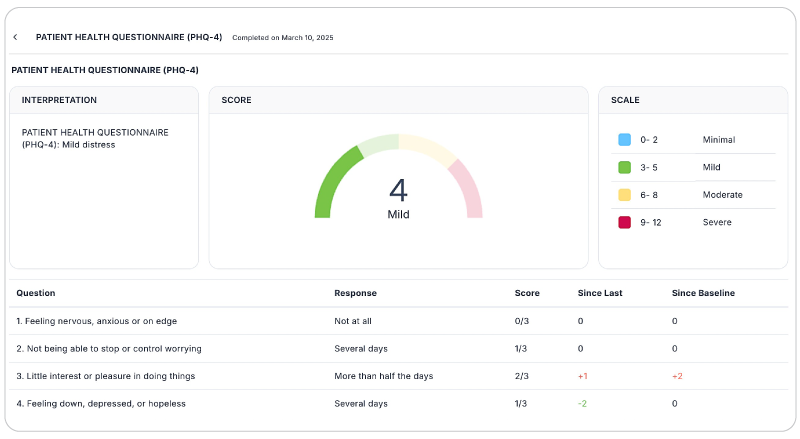
- Whether using CBT, DBT, EMDR, or mindfulness-based practices, clinicians should align techniques with client needs and track outcomes using structured tools like the PHQ-9 or SUDS. Using an EHR to automatically score outcome measures can lead to higher accuracy in less time.
- Avoid generalizations, assumptions, and jargon. Use behavioral observations, client-reported metrics, and outcome scales to show progress and enhance the clinical value of each session note.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Whether you're a clinician, counselor, social worker, or intern learning the ropes, accurately recording therapeutic interventions is not only a best practice, it's a necessity.
Proper documentation improves treatment outcomes, supports continuity of care, and protects both practitioner and client in legal and ethical contexts.
But what exactly counts as a therapeutic intervention? And how can we ensure that documentation is clear, measurable, and clinically useful?
Let's explore key definitions, the importance of proper documentation, commonly used interventions, and get expert tips to use in your practice.
What are therapeutic interventions?
Therapeutic interventions are structured techniques or strategies used by mental health professionals to address specific psychological issues or symptoms.
They are tailored to meet the client's goals outlined in their treatment plan and grounded in theoretical frameworks and evidence-based practices.
They may range from cognitive strategies to emotional processing, behavioral change, or somatic regulation. Importantly, the chosen interventions must align with the client's diagnosis, stage of treatment, and individual preferences.
According to the American Psychological Association (APA), evidence-based interventions are expected and required in most clinical settings to ensure ethical and effective care.
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

Common therapeutic interventions
Let's examine some of the most commonly used and evidence-supported therapeutic interventions, their entailments, and the conditions they benefit most from.
Cognitive Behavioral Therapy (CBT)
CBT is one of the most researched and widely applied therapy interventions. It identifies and restores distorted thinking patterns to affect emotional regulation and behavior. It is structured and goal-focused and often includes worksheets, behavioral experiments, and journaling exercises.
- Best for: Depression, anxiety disorders, PTSD, OCD, eating disorders, and insomnia.
- Intervention example: Challenging automatic negative thoughts using a thought record worksheet.
- Documentation: "Client completed CBT thought log identifying three automatic negative thoughts and associated cognitive distortions (catastrophizing and black-and-white thinking). Successfully restructured beliefs using Socratic questioning. The clinician observed increased insight and reduced defensiveness during the session. Assigned homework: daily thought record for tracking negative thoughts and alternative responses."
Dialectical Behavior Therapy (DBT)
DBT combines CBT with mindfulness, emotion regulation, distress tolerance, and interpersonal effectiveness. Sessions are typically highly structured and often involve skills training groups, diary card tracking, and validation strategies.
- Best for: Borderline Personality Disorder, mood disorders, PTSD, and eating disorders.
- Intervention example: Practicing distress tolerance skills (e.g., TIP skills) during a session on emotional crises.
- Documentation: "Engaged in DBT skill-building focused on distress tolerance. The client practiced paced breathing, TIP temperature change, and grounding techniques in-session. Reported initial SUDS of 7/10 reduced to 4/10. Clinician observed physical relaxation and decreased vocal tension. Homework assigned: complete diary card tracking distress episodes and effectiveness of coping skills."
- Intervention example: Practicing distress tolerance skills (e.g., TIP skills) during a session on emotional crises.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is a structured eight-phase trauma therapy that uses bilateral stimulation (e.g., eye movements, tapping) to help clients process distressing memories and reduce reactivity.
- Best for: PTSD, trauma-related disorders, anxiety, and some phobias.
- Intervention example: Phase 4 reprocessing of a specific traumatic event using bilateral eye movements.
- Documentation: *"Conducted EMDR Phase 4 reprocessing targeting early childhood medical trauma. Bilateral stimulation utilized via tactile buzzers. Client reported vivid recall, followed by emotional release and cognitive shift ('It wasn't my fault'). SUDS decreased from 6 to 2. Clinician noted tearfulness, followed by calm affect and improved grounding. Homework: journaling on positive belief 'I did the best I could' and incorporating a calming evening routine with bilateral stimulation (e.g., bilateral tapping) to reinforce integration. Plan to reassess memory target and emotional response in the next session.
- Intervention example: Phase 4 reprocessing of a specific traumatic event using bilateral eye movements.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

Mindfulness-Based therapy
This approach integrates mindfulness meditation, present-moment awareness, and nonjudgmental observation of thoughts and emotions. It is often used as part of Mindfulness-Based Stress Reduction (MBSR) or Mindfulness-Based Cognitive Therapy (MBCT).
- Best for: Anxiety, depression, chronic pain, and stress-related disorders.
- Intervention example: Guided 5-minute mindful breathing exercise during session.
- Documentation: "Client engaged in guided mindfulness breathing exercise. Reported shift from 6/10 to 3/10 on subjective stress scale. Clinician observed slowed speech, improved posture, and increased verbal reflection. Discussed the concept of 'thoughts as passing clouds.' Assigned daily 10-minute body scan audio practice and journaling reflections on mindfulness experience.
- Intervention example: Guided 5-minute mindful breathing exercise during session.
Exposure Therapy
Exposure therapy helps clients confront fears safely and control them through graduated exposure. This process reduces avoidance behavior and fear reactivity.
- Best for: Phobias, PTSD, OCD, panic disorder.
- Intervention example: In-session exposure hierarchy for driving-related anxiety.
- Documentation: "Client completed second step in exposure hierarchy: viewing videos of freeway driving. Initial anxiety reported as 8/10, reduced to 5/10 by session's end. Client noted surprise at reduced physical tension. Clinician observed reduced fidgeting and improved verbal fluency mid-task. Homework: record thoughts and SUDS levels while sitting in a parked car at a familiar location. Next session to address step three in hierarchy."
- Intervention example: In-session exposure hierarchy for driving-related anxiety.
Solution-Focused Brief Therapy (SFBT)
SFBT emphasizes solutions over problems by identifying past successes, setting goals, and utilizing brief, goal-oriented conversations. It avoids digging into pathology and focuses on strengths and resources.
- Best for: Adjustment disorders, life transitions, mild depression or anxiety.
- Intervention example: Identifying "exceptions" to problem behavior and constructing solutions.
- Documentation: "Utilized SFBT techniques to identify exception moments when client effectively managed work stress. Client expressed confidence and pride recalling past success. Clinician noted shift in posture and affect (more upright, smiling). Homework assigned: write down two daily actions that align with the client's preferred future. Plan to co-create a goal ladder next session."
- Intervention example: Identifying "exceptions" to problem behavior and constructing solutions.
Narrative Therapy
Narrative Therapy helps clients reframe their experiences by exploring the stories they tell about themselves. Through externalization and re-authoring, clients are empowered to shift identity and meaning.
- Best for: Identity issues, trauma, cultural and social issues, family conflict.
- Intervention example: Externalizing the problem to shift narrative control to the client.
- Documentation: "Narrative intervention utilized to externalize 'Anxiety Monster' from client's identity. Client reported feeling less blame and more agency over emotional experience. Clinician observed increase in metaphor use and creative expression. Assigned journaling task: write a dialogue between self and 'Anxiety Monster' to explore influence and strategies for resistance. Next session to focus on mapping influence of the problem."
- Intervention example: Externalizing the problem to shift narrative control to the client.
How to properly document therapeutic interventions
Documentation is the bridge between clinical action and continuity of care.
A well-written intervention note allows another provider – or your future self – to understand what happened in the session, why it happened, how the client responded, and what comes next.
Strong notes support ethical practice, effective treatment planning, and insurance reimbursement. Most clinicians use SOAP, DAP, or BIRP notes to document therapeutic interventions. Each format offers a consistent way to organize session content and clinical decisions:
SOAP (Subjective, Objective, Assessment, Plan)
- Subjective (S): Client's self-report, including symptoms, emotions, or experiences.
- Example: "Client reported feeling 'on edge all week' with increased irritability and difficulty sleeping."
- Objective (O): Clinician observations and measurable findings.
- Example: "Client appeared fatigued, avoided eye contact, and scored 15 on the PHQ-9."
- Assessment (A): Clinician's clinical impressions and synthesis.
- Example: "Client's symptoms consistent with moderate depression; stress related to upcoming work deadline contributing to symptom increase."
- Plan (P): Future steps, homework, referrals, or next session goals.
- Example: "Plan to continue CBT, focus on restructuring negative thoughts; assign sleep hygiene log."
Where to include interventions: The "O" (Objective) section is often where you note specific interventions, or you may expand on them in the "A" if discussing client response.
DAP (Data, Assessment, Plan)
- Data (D): Combination of subjective and objective data.
- Example: "Client reported panic symptoms during a recent work meeting. Observed shallow breathing and clenched fists. Completed in-session grounding technique with visible relaxation."
- Assessment (A): Your interpretation and clinical understanding.
- Example: "Client continues to benefit from somatic interventions; shows growing insight into anxiety triggers."
- Plan (P): What's next, including clinical goals, homework, or follow-ups.
- Example: "Client will continue daily practice of 5-4-3-2-1 technique. Will address core beliefs about public speaking in next session."
Where to include interventions: The "D" section captures what was done and how it was received. Use the "A" to add context.
BIRP (Behavior, Intervention, Response, Plan)
- Behavior (B): What the client presented with during the session.
- Example: "Client appeared withdrawn, spoke softly, and expressed feelings of hopelessness."
- Intervention (I): What you did during the session.
- Example: "Utilized CBT techniques to challenge black-and-white thinking; introduced activity scheduling worksheet."
- Response (R): How the client responded to the intervention.
- Example: "Client engaged with moderate interest, expressed difficulty identifying enjoyable activities but was able to list three."
- Plan (P): Follow-up and clinical direction.
- Example: "Client will complete activity scheduling worksheet daily and bring it to next session. Plan to process outcomes and evaluate motivation."
Where to include interventions: BIRP specifically gives the "Intervention" its own space, making it ideal for detailing your methods and client reactions.
Watch this video to learn how to save time on therapy notes
Documentation tips for therapeutic interventions
- Be specific. "Discussed anger" isn't enough. What intervention was used? What was the client's response?
- Keep it clinically relevant. Focus on what was done in the session and why.
- Avoid jargon. Assume other professionals (and clients) may read the notes.
- Don't skip the response. Client engagement level and reaction matter.
- Use templates and checklists for consistency.
What to avoid when documenting therapeutic interventions
- Overgeneralizations: "Talked about week" provides no therapeutic insight.
- Assumptions: Document what the client said and did, not what you think they felt.
- Omissions: If you used a modality, name it. Record any strong reaction from a client.
- Unmeasured progress: Use scales or client-reported outcomes where possible.
Therapeutic interventions are the heartbeat of effective mental health care. They must be intentionally chosen, tailored to the individual, and documented with care. Using clear, structured documentation and evidence-based strategies elevates the quality of care—it protects the client, the provider, and the integrity of the therapeutic process.
Keep a reference list of interventions handy and revisit your documentation process regularly to ensure it meets ethical, clinical, and insurance standards.
Make outcomes measurable and clinically relevant
Avoid generic or vague language like "talked about anxiety" or "worked on goals." Instead, frame the intervention clearly, tie it to the treatment plan, and show results. Use:
- Client-reported outcomes: "Client rated anxiety at 8/10 at session start; post-intervention, reported reduction to 4/10."
- Structured tools: Incorporate assessment tools (GAD-7, PHQ-9, SUDs scale, etc.) regularly and note scores to show progress or need for adjustment.
- Behavioral observations: Document what you actually saw and heard: "Client became tearful but remained engaged; demonstrated new insight into relationship patterns."
Answer the three big questions in the intervention therapy note
What did you do?
- "Used Socratic questioning to explore automatic thoughts about self-worth."
- "Led client through guided imagery to create a calming 'safe space.'"
Why did you do it?
- "To challenge cognitive distortions contributing to depressive symptoms."
- "To help the client regulate, affect and reduce physiological arousal."
How did the client respond?
- "The client expressed resistance initially but engaged after clarification. Reported sense of relief after visualization."
- "Client was highly engaged and verbalized a sense of empowerment."
Consider including homework or between-session plans
Documenting take-home assignments supports accountability and encourages skill generalization:
- "Assigned daily journaling on cognitive distortions using thought log."
- "Client will practice DBT emotion regulation skills daily and track outcomes."
- "Referred client to EMDR video on safe place exercise for daily use."
Improving therapy notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly.
This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs.
However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style.
This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.
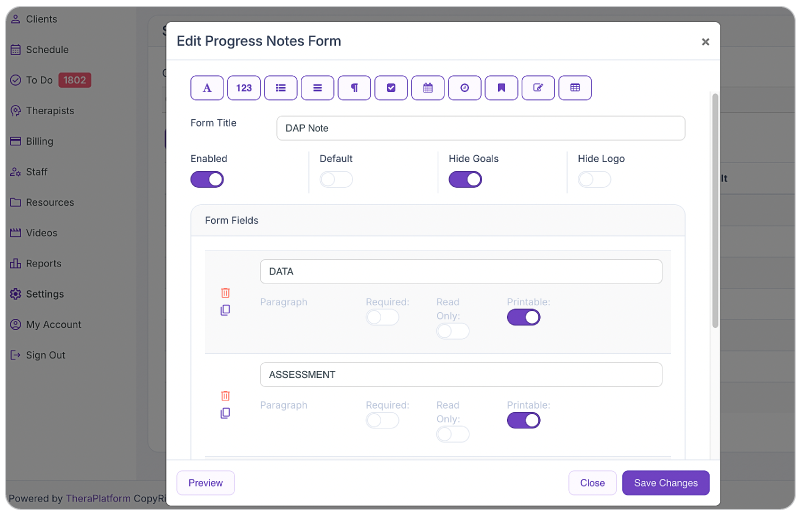
Screenshot of TheraPlatform’s notes form builder. Easily complete notes based on templates and update for the specific needs of the session.
- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information.
- TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes.
- Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.
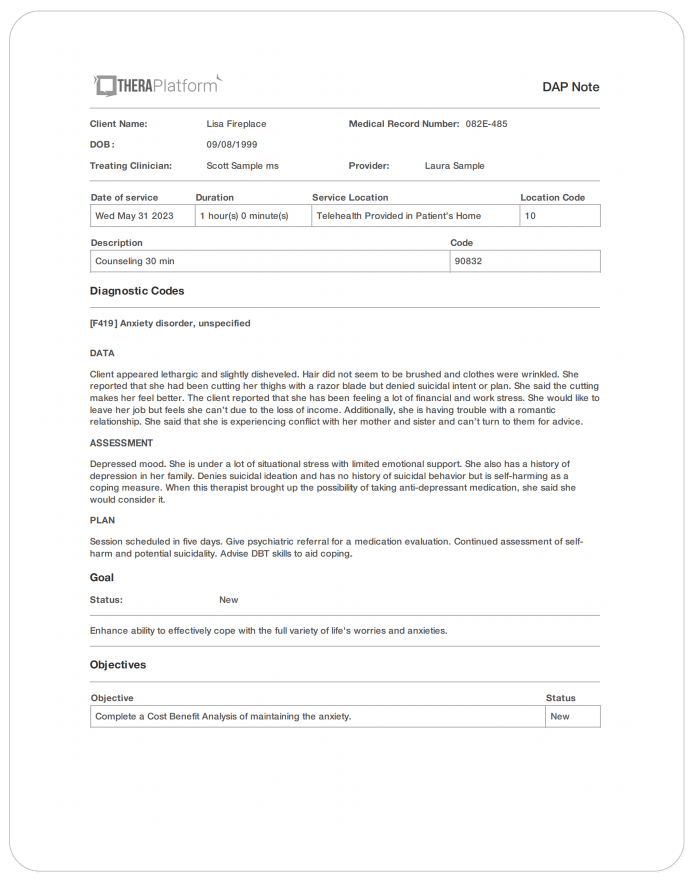
Screenshot of TheraPlatform’s notes template
- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time.
- This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures.
- TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services.
This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Additional tools and outcome measures to help with data collection and progress monitoring
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session.
The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
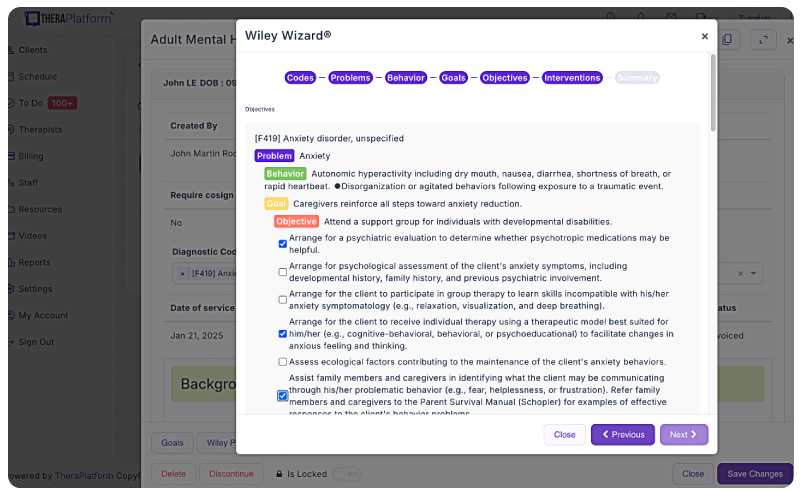
Screenshot of Wiley Treatment Planner integration into TheraPlatform illustrating how areas like problems, behaviors, goals and objectives can be completed with pre-populated, research-based statements.
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually. However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatfrom automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
Screenshot of TheraPlatform’s outcome measures page
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools
Free video classes
- Free on-demand insurance billing for therapist course
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice
References
American Psychological Association. (2023). Evidence-Based Practice in Psychology. https://www.apa.org/practice/guidelines/evidence-based-statement
Linehan, M. M. (1993). Cognitive-Behavioral Treatment of Borderline Personality Disorder. The Guilford Press.
Shapiro, F. (2018). Eye Movement Desensitization and Reprocessing (EMDR) Therapy: Basic Principles, Protocols, and Procedures (3rd ed.). Guilford Press.
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2018). Mindfulness-Based Cognitive Therapy for Depression (2nd ed.). Guilford Press.
Beutler, L. E., Harwood, T. M., Kimpara, S., & Malik, M. (2011). Evidence-Based Practices for Mental Health Professionals: A Supplement to the APA Dictionary of Psychology. APA.
de Shazer, S., & Dolan, Y. (2007). More Than Miracles: The State of the Art of Solution-Focused Brief Therapy. Routledge.
White, M., & Epston, D. (1990). Narrative Means to Therapeutic Ends. Norton & Company.
National Institute for Health and Care Excellence (NICE). (2011). Generalised anxiety disorder and panic disorder in adults: Management. https://www.nice.org.uk/guidance/cg113
Oxford Mindfulness Foundation. (n.d.). Home of MBCT research. Oxford Mindfulness Foundation. https://www.oxfordmindfulness.org
Institute for Solution-Focused Therapy. (n.d.). Solution-focused brief therapy resources and training. https://solutionfocused.net
EMDR International Association. (n.d.). About EMDR therapy. https://www.emdria.org/about-emdr-therapy
Behavioral Tech. (n.d.). Dialectical behavior therapy (DBT) – FAQs. https://behavioraltech.org/resources/faqs/dialectical-behavior-therapy-dbt
FAQs about therapeutic interventions and documentation
What counts as a therapeutic intervention?
A therapeutic intervention is a structured, evidence-based technique or strategy (e.g., CBT, DBT, EMDR, mindfulness) used by clinicians to address specific client goals and symptoms outlined in the treatment plan.
Why is documenting interventions so important?
Accurate documentation ensures ethical treatment, supports continuity of care, demonstrates progress, and provides the detail insurance companies require for reimbursement.
What’s the best way to document therapeutic interventions?
Use structured note formats like SOAP, DAP, or BIRP to clearly capture what was done, why it was done, and how the client responded. Avoid vague statements—be specific, measurable, and clinically relevant.