Mental status exams

Mental status exams were one of the first mental health assessment measures. Although the origin of it is not entirely clear, Adolf Meyer is often credited with the ideas behind its creation. In 1918, he developed a rough method to evaluate a patient’s mental state for his psychiatric practice. Since that time, the mental status exam has been refined for a variety of uses, most frequently to measure a person’s cognitive functioning.
Summary
- The Mental Status Exam (MSE) is a clinician-led assessment that uses verbal questions and observations to evaluate a client’s mood, cognition, speech, behavior, and overall functioning at a specific point in time.
- MSEs are flexible but not standardized, allowing clinicians to tailor questions to the individual or setting—but this also limits their reliability and psychometric strength.
- Core components include appearance, mood, affect, thought content, cognition, insight, and judgment—providing a snapshot of mental health that can aid in clinical decision-making.
- The MSE is most commonly used in psychiatric, emergency, or neuropsychological settings—not as frequently in outpatient therapy—though it remains a useful tool across various disciplines. Download your free anxiety worksheets.
- By using an EHR like TheraPlatform, mental health professionals can easily track and manage assessments.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

What is a mental status exam?
The mental status exam (MSE) is administered verbally by a clinician. It involves a series of specific questions—along with therapist observations—that are used to determine the client’s mental state. It intends to measure aspects of cognition, mood, and behavior to form an overall picture of the client at a particular moment. The mental status exam is not standardized. Instead, the clinician can choose what types of questions to ask that will meet their specific objectives. For example, a neuropsychologist working with potential dementia clients might focus more on cognitive processes than their effect.
Components of a mental status exam
The mental status exam is made up of several components.
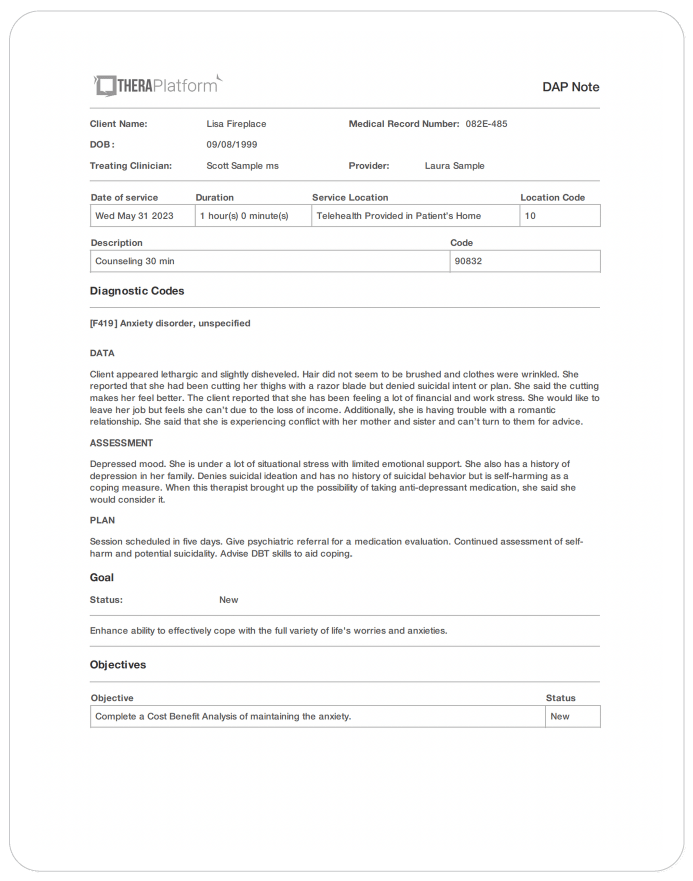
Appearance
This category provides an overall physical impression of the client. Are they well-groomed and neatly dressed? How is their posture? Do they have a foul odor? You don’t want to judge a book by its cover but you can often tell a lot about a person by their appearance. If a client shows up for an appointment looking disheveled, it tells you something about their functioning.
Behavior
Similarly, a client’s behavior during a mental status exam can give you clues as to their behavior outside the office. Are they cooperative? Do they have good eye contact? Do they exhibit agitation or irregular movements?
Mood
Mood is how the client perceives their current internal emotional status. Therefore, a simple question from the clinician, such as “How do you feel today?” can give you a glimpse into a client’s mood.
Affect
Affect, in contrast, is how a client’s emotional state is perceived by the therapist. A clinician observes body movements, facial expressions, and speech, among other factors, to determine a client’s affect.
Speech
Much can be ascertained about a person from their speech, including symptoms of anxiety and problems with cognition. For example, is it clear or slurred? Is it pressured or relaxed? Asking open-ended questions can give the therapist a good idea of the client’s natural speech fluency.
Thought content
This category helps determine what a client is thinking about. Thought content can give indications about serious problems, including suicidal ideation, hallucinations, delusions, and obsessive thinking. For instance, a therapist might ask, “Do you ever see things that other people don’t see?
Thought Process
Thought process, on the other hand, has to do with the rate of thoughts and how they are connected. For example, when asked a question, does the client provide a coherent answer in an appropriate time frame? Or are they rambling and going off on tangents? Do they have racing or fragmented thoughts?
Cognition
Cognition includes orientation to time, place, person, and situation (i.e., What is today’s date? Where are you? Who are you? What are you doing here?). It also includes memory and the ability to concentrate. For example, the clinician might ask the client to remember a series of seven numbers and then repeat the numbers back to them. Or the therapist may go back later in the interview to see if the client still remembers, to test long-term memory.
Judgment
Questions of judgment assess whether a person acts appropriately in a given situation. For example, a client may be asked, “What would you do if you saw the person ahead of you drop a $20 bill?” Besides hypothetical situations, it is also beneficial to explore situations that have already occurred and may have had negative consequences: “How would you handle your situation now if you had another chance?”
Insight
Insight involves the level of understanding the individual has about themselves and their problems. In other words, do they understand the reality of their situation and what is necessary to help them improve? Insight is an integral part of the success of treatment. In general, poor insight leads to an unfavorable prognosis.
For a more detailed exploration of the components of the mental status exam, you can check out this informative worksheet.
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

When should I use the mental status exam?
Whether or not a clinician administers a mental status exam often depends on their profession. For example, an MSE is a common part of a psychiatric evaluation but not as popular with outpatient psychotherapists. That may be because it tends to feel more medical.
This is not to say that a therapist would never give an MSE, but they generally have their own intake forms and are more concerned with past behavior, presenting problems, and individual goals as compared to how a client is functioning at a particular point in time.
Therefore, if someone presented at an emergency room for a mental health issue, the clinician would probably perform an MSE, but a client would not as likely receive one as part of a psychotherapy intake session.
Additionally, the MSE is often used as a screening measure for neuropsychological impairment and is performed more with elderly populations or those with suspected brain deficits. You will find it administered less to clients with traditional therapy concerns, such as depression or anxiety.
Having said that, a clinician may perform a mental status exam with any client in any setting. It provides a lot of useful information. The MSE often gives you the first glimpse of the symptoms that make up psychiatric disorders.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

Is a mental status exam a valid and reliable measure?
A mental status exam can provide valuable information about a person’s mental state at a particular moment in time. However, it is not a highly valid or reliable measure. This is mainly because it is not standardized. The MSE given in a hospital, for instance, may be very different from the one given in a psychiatrist’s office. It should be noted that this is also a strength of the MSE. It can be tailored for a particular client or population. Just don’t look at a mental status exam as an example of strong psychometric assessment properties.
What is the mini-mental state exam?
The Mini-Mental State Exam (MMSE) is a standardized assessment tool that measures the severity of cognitive impairment over time. It is only 11 questions and is used as a screening item for cognitive difficulties. Despite sharing a similar name, it is not to be confused with a mental status exam. Although both measures can assess cognitive deficits, the MMSE has an isolated focus and exhibits stronger psychometric properties.
Resources for further study
The following resources can be used to enhance your understanding of a mental status exam:
- The Mental Status Examination Handbook provides all the information you need to become an expert in administering mental status exams.
- Positive Psychology has an informative piece on mental status exams and gives an example of a mental status exam done with both a child and an adult.
- Some clinicians prefer a checklist when administering a mental status exam. This allows for a more concise accounting but, of course, may limit the amount of information received.
Improving mental health assessment notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
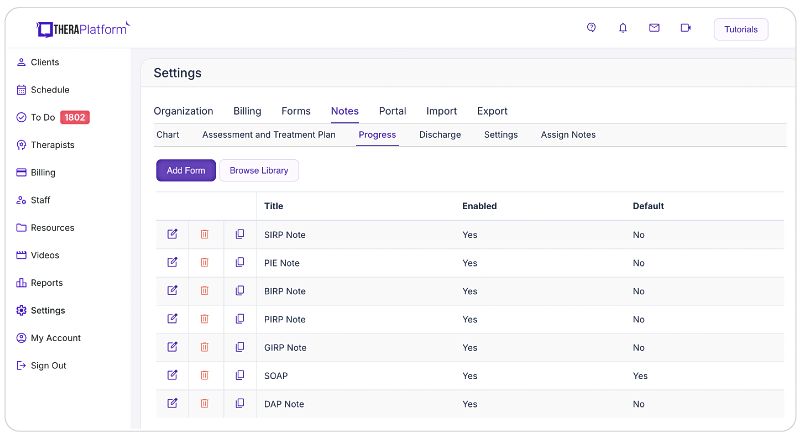
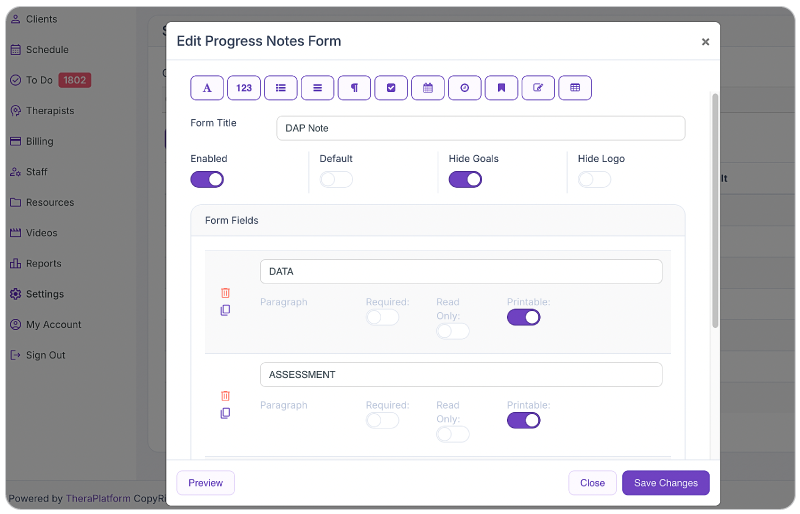
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.
- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.
- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
Additional tools and outcome measures to help with data collection and progress monitoring
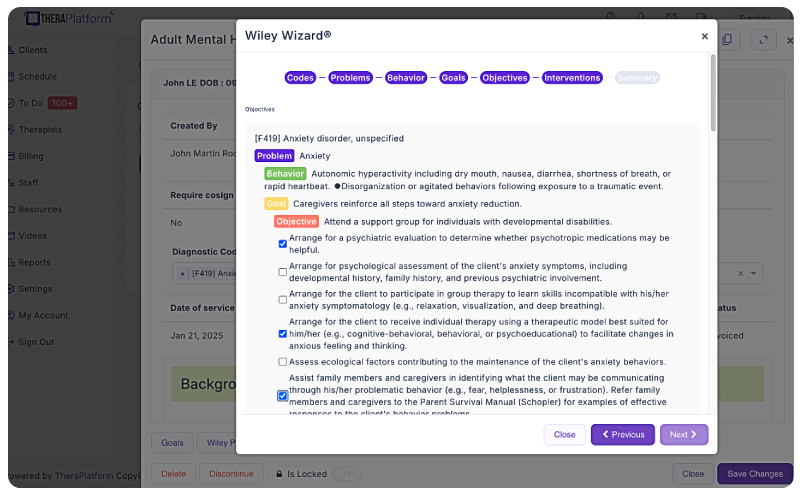
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
Watch this video to learn about how to autoscore outcome measures
→ Sign up for a Free Frial
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually.
However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
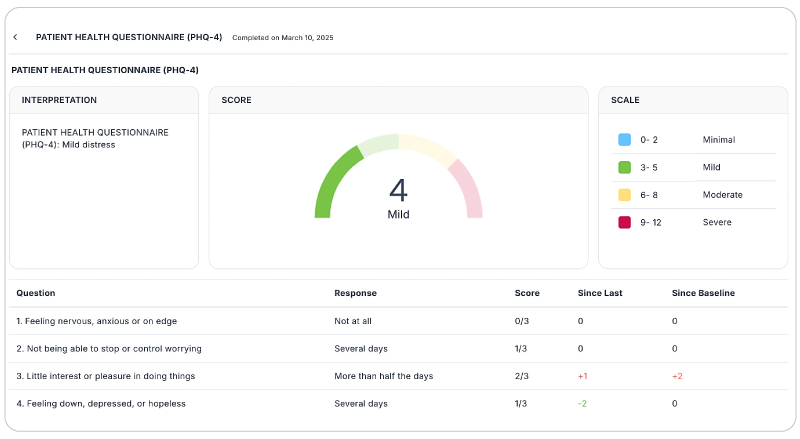
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatfrom automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution with AI-powered note taking that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools



