Mental health assessments

Mental health assessments are used for several different reasons in therapy. Assessments can provide information for diagnosis or to maintain a check on the progress or severity of symptoms. They can reassure clients that they are on the right track and help therapists keep an eye on any potential red flags or warning signs with their client’s condition.
Summary
- Mental health assessments are essential tools for diagnosis, treatment planning, and tracking symptom progress, and can range from brief screeners to in-depth psychological evaluations.
- Common assessments include tools for depression (PHQ-9, BDI), anxiety (GAD-7, BAI), PTSD (PCL-5, CAP-5), and suicidality (Columbia Scale, SAD PERSONS), many of which are freely available and easy to administer. Download my free mental health assessments.
- While helpful, assessments can be affected by client dishonesty, symptom overlap between disorders, and limited predictive power—especially in high-risk areas like suicidality.
- Digital platforms and EHRs can streamline assessment administration and storage, allowing therapists to efficiently monitor client progress and reduce time spent on paperwork.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Psychological evaluation versus mental health assessments
It is important to differentiate between a psychological evaluation and an assessment tool. A full psychological evaluation is a large battery of tests and clinical interviews which collects a plethora of information about the identified client and their situation.
This is then analyzed by a trained psychology professional with a Master’s Degree or Ph.D. Depending on the level of evaluation needed, and a large report with information about the assessment results, interpretation, diagnosis, and treatment recommendations is written. This test battery is likely to include intellectual, achievement, and personality tests that require specific training and licensure to administer and interpret.
This type of evaluation is typically quite thorough, time-consuming, and costly. Evaluations are typically completed over multiple days and take more days to analyze, assemble, and report on. Psychological evaluations need to be done in person as many psychological tests must be completed in person face to face.
Mental health assessments, on the other hand, tend to be more brief and specific. Many of the evaluations we will discuss have 20 or fewer questions and are related to either a specific disorder or are general questionnaires intended to guide the clinician to another assessment for a specific disorder. Assessments are typically self-report in nature and can be completed in person, however, even in person, they are often completed outside of meeting with the clinician, and completing the assessments online is commonplace.
Mental health assessments
Assessments for Depression | Abbreviation |
|---|---|
Patient Health Questionnaire | (PHQ-9) |
Beck Depression Inventory | (BDI) |
Self-Rating Depression Scale | (SDS) |
Assessments for Anxiety | Abbreviation |
Beck Anxiety Inventory | (BAI) |
Generalized Anxiety Disorder-7 | (GAD-7) |
Depression Anxiety Stress Scales | (DASS) |
Assessments for PTSD | Abbreviation |
PTSD Checklist for DSM-V | (PCL-5) |
International Trauma Questionnaire | (ITQ) |
Clinician-Administered PTSD Scale for DSM-V | (CAP-5) |
Assessments for Suicidality and Self-harm | Abbreviation |
Columbia-Suicide Severity Rating Scale | C-SSRS |
SAD PERSONS Scale | |
Self-Harm Inventory | (SHI) |
Mental health assessments for depression
Several mental health assessments or screeners for depression exist. The three discussed here are most commonly used in practices. They are all fairly short and directly ask about typical symptoms of depression in a simple and understandable way. While they all have specific scoring methods, it is easy enough for a clinician to look at the raw answers to the questions and see how the client is functioning that day.
Patient Health Questionnaire (PHQ-9)
The PHQ-9 is a nine-question subset focused on depression from the 3-page patient health questionnaire and was first used in 2001. Originally intended for screening of depression symptoms in a primary care setting, this questionnaire is useful for anyone assessing depression as it is based on the DSM-4 symptoms specific to major depression. Each question has answers that range from 0 (not at all) to 3 (nearly every day). The PHQ-9 also has the advantage of being free and readily available to clinicians. More information about the PHQ-9 can be found in the American Psychological Association’s article.
Beck Depression Inventory (BDI)
The BDI was originally developed in 1961 as an inventory to assess the severity of depressive symptoms. It is a 21-question screener where answers range from not at all to high intensity regarding the client’s symptoms in the past week. The BDI has been modified a few times since its inception and exists in short form and an updated BDI-II form. The BDI requires the purchase of a license for its use and like other self-report forms can be falsified if the individual chooses to be dishonest. It is important to remember that assessments like these are intended to be part of the diagnostic assessment, not used as a sole measure of diagnosis.
Self-Rating Depression Scale (SDS)
The SDS was also developed in the 1960s but is readily and freely available to individuals who wish to use it. It consists of 20 self-report questions related to symptoms of depression where answers range from “none of the time” to ‘most of the time.” Answers are then assigned a number to get the raw score and converted to get the total score. There is also a clinician-rated scale available.
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

Mental Health assessments for anxiety
Anxiety is another area with many assessments available The most common assessments will be covered here, but it’s important to note that a variety of different anxiety disorders and presentations are available. The correct assessment should match the individual’s disorder and symptom presentation.
Beck Anxiety Inventory (BAI)
The BAI is a self-report mental health assessment developed to measure the severity of anxiety. It was developed by pulling information from the PDR checklist, the Anxiety checklist, and the situational anxiety checklist. Analysis was completed repeatedly to decrease from 86 questions to 21 that best represent anxiety. It utilizes a four-point scale to measure how bothered by symptoms the individual has been.
Generalized Anxiety Disorder-7 (GAD-7)
The GAD-7 was originally developed for Generalized Anxiety disorder but is increasingly used for any type of anxiety screening. It is a 7-question screener with answers ranging from not at all to nearly every day. The general nature of the questions allows them to be easily adapted to other anxiety disorders making it an easy way to maintain an accounting of symptom severity.
Depression Anxiety Stress Scales (DASS)
There are two different versions of the Depression Anxiety Stress Scale - a 21-question version, and a 42-question version. Each measures symptoms of depression, anxiety, and stress and their severity. For complex depression affected by symptoms of anxiety and stress, this measure is a great way for clinicians to keep track of symptoms and severity as a measure of how the client is doing and the progress being made. Both versions of the scale are readily available online and easy to use by any mental health professional.
Mental health assessments for PTSD
In the area of mental health, PTSD is an area that has rapidly evolved over the last 100 years from a place of complete ignorance and denial to a place more of acceptance and understanding. This evolution has allowed combat veterans and civilians who have experienced trauma to seek out treatment more readily which has encouraged the development of several assessments for the diagnosis and ongoing monitoring of trauma symptoms.
PTSD checklist for DSM-V (PCL-5)
The PCL-5 is the most updated version of the PTSD checklist. It is a 20-question self-report questionnaire that can be used to screen for PTSD, monitor symptoms and progress before, during, and after treatment, and make a provisional diagnosis of PTSD. It utilizes a 5-point scale and is not time-consuming for the client to complete regularly. This is a freely accessible mental health assessment but should be limited to being interpreted by trained clinicians. More information is available on the VA website.
International Trauma Questionnaire (ITQ)
The ITQ is set up for PTSD and Complex PTSD as defined by ICD-11. It is 18 questions in all, 9 for PTSD and 9 for CPTSD. They are all simply worded and related to diagnostic criteria. The questionnaire uses a five-point Likert scale to measure how much each criteria point has bothered the individual in the past month. Again this measure can be used to screen for PTSD, monitor symptoms and progress before, during, and after treatment, and make a provisional diagnosis of PTSD. It is available along with references, resources, and more information at the ITQ website in a variety of languages.
Clinician-Administered PTSD Scale for DSM-V (CAP-5)
The CAP-5 is specifically geared towards PTSD as defined by the DSM-V. It is clinician-administered and requires specific training, which is easily available on the Veteran Affairs website. Training goes over the questions involved as well as the follow-up/clarifying responses the clinician can use. It can be used to diagnose and assess PTSD in “veteran and civilian trauma survivors.” The VA website touts this as the “gold standard” of PTSD assessment. The longest of the assessments mentioned here, this scale takes approximately 45-60 minutes to complete.
Mental health assessments for suicidality and self-harm
Because suicide is still fairly rare and unpredictable evaluating the threat can be complicated and some methods of assessment have been devised to assist clinicians in this process. The most useful tool in a clinician’s toolbox to assess suicidality or self-harm behaviors is the clinical interview. Most clinicians are thoroughly trained in the series of questions to ask to probe for suicidality and this remains the most effective measure to use.
Columbia-Suicide Severity Rating Scale
The Columbia scale was developed at Columbia University with the University of Pennsylvania, and the University of Pittsburgh and focuses on suicidal ideation as a predictor of suicidal action. The Columbia scale is a brief mental health assessment that can be administered in the field by individuals not trained as mental health professionals in order to determine the next steps to be taken. The scale consists of 6 simple yes or no style questions. The Columbia scale is even available via a free app that can walk an individual through the questionnaire and guide them based on given answers which is available in both the google play store and the Apple app store.
SAD PERSONS Scale
The SAD PERSONS scale is part pneumonic to remember risk factors in suicidality and part scale to recognize the level of risk. It is widely used especially in non-psychiatric settings.
The scale consists of:
- S: Sex male
- A: Age <19 or >45
- D: Depression
- P: Previous attempt
- E: Excessive alcohol or substance use
- R: Rational thinking loss
- S: Social support lacking
- O Organized plan
- N: No partner
- S: Sickness
For each factor that is positive, the clinician should add one point.
3-6 points indicate a follow-up needed
7-10 indicates high risk and the potential need for admission to a hospital.
Self-Harm Inventory (SHI)
The Self-Harm Inventory is a 22-question yes/no inventory of potential self-harm behaviors. It is a self-report mental health assessment and while it is not an exhaustive list of potential behaviors, it is fairly comprehensive. As with suicidality, a clinical interview is typically the best policy for understanding the severity of behaviors, however, at times when a quick screener is needed, the SHI is a short and simple measure with benefit.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

Potential problems with mental health assessments
While mental health assessments have a variety of uses, some potential problems and drawbacks exist.
Dishonesty is a problem that is potentially an issue with any reported symptoms. While more advanced psychological testing has values that differentiate between individuals that are being honest and individuals that are not being honest, basic screeners and assessments have nothing to validate the honesty level of the individual. The biggest risk is individuals “faking good,” particularly with screeners for suicidality and hiding negative symptoms from clinicians.
Individuals endorsing worse symptoms than they are actually experiencing is a risk too. However, this exaggeration can be explored in therapy if the clinician finds that the self-report doesn’t match the presentation in person. Many reasons can exist behind the exaggeration of symptoms, but each one of them provides important information to the clinician about the individual, therefore, there is benefit in assessment.
The ambiguous nature of mental health disorders also makes assessment difficult. Many disorders have overlapping symptoms or presentations and there is no blood test for mental health disorders like physical health disorders. Assessments for depression often ask about difficulty concentrating which could come from attention disorders as one example.
Additionally, some assessments lack consistent evidence of validity. For example, most assessments of suicidality often lack consistency in predicting those individuals who follow through with suicide. In fact, some assessments of depression and hopelessness are better at predicting suicide than suicidal assessments.
Challenges of assessing online
Many mental health assessments can easily be used online as effectively as they are in person. A majority of the assessments discussed above are self-reported, and when done in person may not even be completed in front of the clinician.
Additionally, many mental health assessments cannot be completed online. Intelligence tests and projective tests have to be conducted in person or through telehealth and some assessments need behavioral observations.
Benefits of using mental health assessments
While there are some negatives to using mental health assessments in treatment, there are benefits like allowing progress to be monitored and assisting in diagnosis. A significant benefit of mental health assessments is the ability to quantitatively measure progress in treatment. When assessments are given at the beginning of treatment to measure the severity of symptoms and periodically throughout treatment then both client and provider can visually see the progress being made.
Additionally, mental health assessments can give a name to what is going on. The unknown in treatment is the worst feeling that most people ever experience. Having a name and an idea of what to do about it can be a relief to the patient who has been suffering from symptoms and not knowing what to do about it. Suffering and dealing with confusion and frustration can often feel so much worse than finally having an answer.
Improving mental health assessment notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
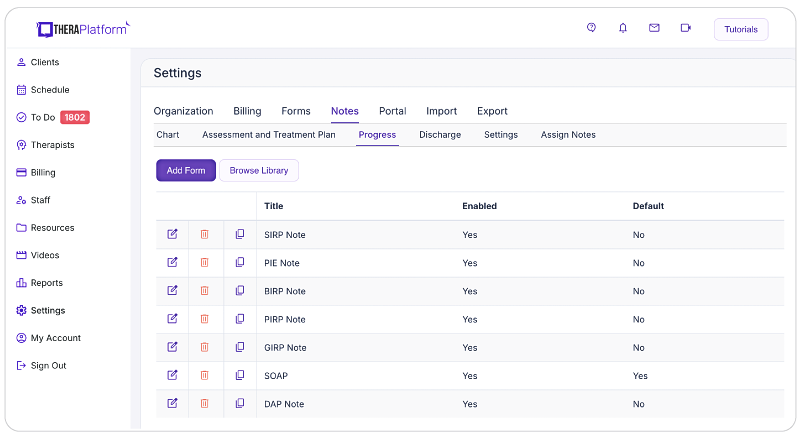
Screenshot of TheraPlatform’s built-in therapy note template library. Notes are one of dozens of types of templates that can be used as is or modified to meet the needs of a therapist in private practice
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.

- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.

- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
Additional tools and outcome measures to help with data collection and progress monitoring
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
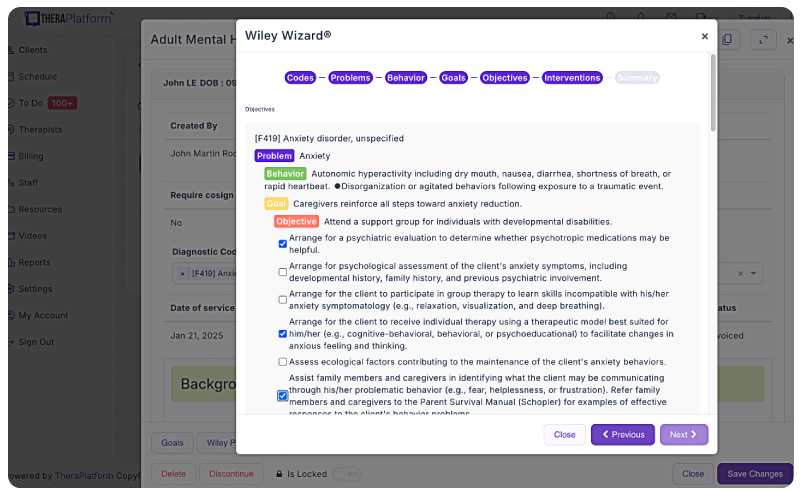
Screenshot of Wiley Treatment Planner integration into TheraPlatform illustrating how areas like problems, behaviors, goals and objectives can be completed with pre-populated, research-based statements.
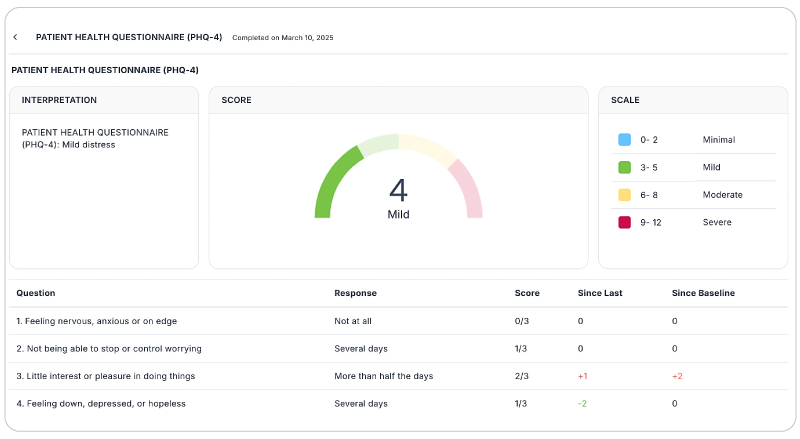
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
Watch this video to learn about how to autoscore outcome measures
→ Sign up for a Free Frial
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually.
However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatfrom automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution with AI-powered note taking features that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools



