Depression assessments

Depression assessments are used to assess one of the most common and debilitating mental health disorders – depression. Approximately 9.5 percent of American adults have a depressive illness each year.
Summary
- Depression assessments guide accurate diagnosis and treatment, helping clinicians select appropriate modalities like CBT, DBT, or EMDR.
- Validated screening tools such as the PHQ-9, BDI-II, CES-D, and clinician-administered scales (HAM-D, MADRS) are essential for consistent assessment. Download my free depression tests.
- Reassessment is criticalas repeated evaluations help measure progress and adjust care plans over time.
- Suicide risk screening is a vital step in depression assessment, often using tools like the C-SSRS and SBQ-R.
- Using EHR systems such as TheraPlatform can significantly streamline tasks like outcome measures and documentation.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

And those who do often suffer serious consequences. It is estimated that 11.4 percent of people visiting hospital emergency rooms in the United States each year are due to depression.
Because of its prevalence and severity, accurate depression assessments are crucially important.
In this article, we will seek to better understand depression, depression assessments and assessment, and how therapists translate diagnosis into treatment.
What is depression?
Depression is a multifaceted disorder that affects emotional, physical, and cognitive functioning. It impacts simple everyday tasks and results in a gradual deterioration of quality of life. Its causes are believed to be both genetic and environmental.
Symptoms of Depression
Here are some of the most prevalent depression symptoms:
Core symptoms of depression
- Persistent sadness or poor mood
- A loss of interest or pleasure in activities that were previously found interesting
- Fatigue or low energy
Other symptoms of depression
- A significant change in behavior of any type. For example, work or school performance may significantly worsen
- An increase or decrease in appetite and/or sleep
- Difficulty concentrating
- Social withdrawal
- Lack of motivation
- Feelings of hopelessness
- Pessimism about the future
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

Types of depressive disorders
Major depression
This is also called clinical depression, and it is what most people are referring to when they talk about depression. According to the International Classification of Diseases (ICD-10), to be diagnosed with major depression, you must have one core symptom for at least two weeks and two or three (or more) other symptoms for at least a month. It is classified as mild, moderate, or severe, depending on the number of symptoms experienced.
Bipolar Depression
People may make a distinction between bipolar depression and major (or unipolar) depression, but they share the same symptoms. In most types of bipolar disorder, there is a period of mania alternating with a depressive episode. These depressive episodes are very similar to major depression. They just happen within a bipolar cycle.
Persistent Depressive Disorder
Otherwise known as dysthymia, this is a form of depression that occurs for at least two years. You may feel some relief over that span but it is fleeting. It is not as severe as major depression, but the individual likely experiences a sad mood and maybe another depressive symptom or two.
Seasonal Affective Disorder (SAD)
During the winter months, certain people might experience depressive symptoms that they don’t experience at other times of the year. The exact causes are speculative but SAD appears to be due to a variety of possible factors (e.g., decreases in vitamin D and serotonin). Although rare, it is possible to experience SAD during the summer months.
Depression assessments
The following are some of the most frequently used depression assessments:
Unstructured interview
Despite an abundance of depression screening tools, the most commonly used way to assess depression is through an unstructured interview. This may occur during intake or in the beginning stages of therapy.
In essence, therapists use their knowledge of depressive symptomatology to elicit the necessary information to formulate a diagnosis. When the client is not forthcoming or presents a more complex diagnostic picture, the therapist may proceed to use self-report or clinician-administered resources.
Self-report tools
These types of resources are self-administered by the client and rely on self-report. They are subject to client honesty and self-awareness, and, for that reason, their validity may be questioned.
The Beck Depression Inventory (BDI-II)
The BDI-II is a 21-item multiple-choice screening tool that covers several aspects of depression. Respondents rate the intensity of each symptom based on their experiences over the past two weeks. It has good reliability and validity; however, the BDI’s reliance on physical symptoms may artificially inflate scores when used with individuals with physical health conditions.
Patient Health Questionnaire-9 (PHQ-9)
The PHQ-9 is the most commonly used depression screening method. It can be used as a standalone tool but it is also a component of the larger PHQ. Respondents rate the frequency of their symptoms over the past two weeks on nine items, providing a quick snapshot of their emotional well-being. Each item is rated according to severity, with scores of 10 or above indicating moderate to severe depression.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D is a 20-item assessment that measures the frequency of depressive symptoms in the past week. Its items encompass a broad range of emotional and behavioral indicators of depression. Originally developed for research purposes, it has become popular in clinical settings. It provides a cutoff score of 16 to identify individuals at risk for clinical depression.
Clinician-administered depression assessments
The following two rating scales must be administered by a trained clinician:
Montgomery-Asberg Depression Rating Scale (MADRS)
The MADRS includes 10 items rated on a six-point scale.It is noted for its sensitivity to changes in depression levels over time. Answers to the items are elicited from the individual through a clinician interview. Scores of 20 or higher indicate moderate to severe depression. The interview style allows the clinician some latitude in exploring the items in more depth.
Hamilton Depression Rating Scale (HAM-D)
The Hamilton Depression Rating Scale was the first depression screening tool.
It contains 21 items, but scores are calculated based on the first 17 items. The last four items are used to provide additional clinical information. Scores over 14 indicate moderate to severe depression. It has been criticized for focusing on physical symptoms, such as insomnia, at the expense of cognitive and emotional factors.
Identifying suicide risk
When depression is severe and suicide risk is suspected, a suicide assessment may be conducted. Clinicians will perform an interview to look for intent, plan, method, and preparation in determining whether the suicide threat is serious.
They may also use the following formal assessment tools:
Columbia-Suicide Severity Rating Scale (C-SSRS)
The C-SSRS is a set of six questions that gauges the seriousness of a person’s suicide risk. The questions increase in severity from low to high risk. Therapists must seek immediate assistance when high-risk questions are answered in the affirmative.
The Suicide Behaviors Questionnaire-Revised (SBQ-R)
The SBQ-R is a four-item screening measure that assesses four dimensions of suicidality, including the likelihood of future suicide attempts. A score of seven or above is cause for concern and may necessitate immediate intervention.
Note: For clients with active suicidal intent, a safety plan is to be implemented.
Translating depression test results into treatment intervention
Accurate diagnosis of depression is only part of the battle. Following through with the appropriate intervention and regular reassessment is necessary for effective treatment.
Selecting appropriate therapeutic modalities
Not every treatment modality is going to work the same with all types of depression. Certain types of therapy may be more effective than others. For example, cognitive-behavioral therapy (CBT) is the gold standard treatment for depression.
However, if someone has a history of suicidal behavior, you may want to try dialectical behavioral therapy (DBT) because it focuses on improving distress tolerance, impulse control, and emotional dysregulation.
Or, maybe someone is depressed because they experienced trauma. In that case, EMDR might be the most effective therapy to deal with their emotions regarding past events. Assessment gives clues as to depression’s sources and severity, and clinicians should choose treatment options accordingly.
Periodic reassessment
Depression assessment is an ongoing process that may require therapists to give diagnostic tools more than once at different intervals. This reassessment enables them to gauge an individual’s progress and address changes in behavior. An improvement in scores will also help motivate clients to continue their efforts. Depending on the results, clinicians may need to tweak the client’s treatment plan to meet their psychological needs.
Why depression assessments matter
Depression assessments are a vital part of the overall treatment process.
It contributions are many:
- Accurate and early diagnosis is associated with improved outcomes and relapse prevention.
- Diagnostic assessment informs treatment planning.
- Assessment results establish a baseline for tracking progress.
- Improvement motivates clients to maintain positive growth.
- Screens for suicide risk and behavior.
Depression assessments are both an art and a science. Clinicians use a combination of formal screening tools and professional experience to produce accurate diagnoses of depressive disorders and choose appropriate modalities for treatment.
Depression can have grave consequences and it is not to be taken lightly. It is encouraging that therapists possess the necessary resources for effective diagnosis.
Documenting depression
An essential component of depression (and indeed nearly all therapeutic work) is accurate, timely documentation.
One common structure is the SOAP format:
- S (Subjective): What the clients report — emotional state, concerns, events since last session.
- O (Objective): What the therapist observes — interaction patterns, tone, nonverbal cues.
- A (Assessment): Therapist’s clinical interpretation — what the subjective and objective data suggest in terms of attachment needs, emotional blocks, and relational dynamics.
- P (Plan): What will be done going forward — interventions, new homework, focus for next session.
SOAP Note – Depression
Client: Jane D.
Date: 10/13/2025
Session #: 5
Diagnosis: Major Depressive Disorder, moderate (F32.1)
Therapist: [Name], LCSW
S – Subjective
Client reports continued low mood and fatigue but notes “slightly more motivation” to complete daily tasks this week. She states, “I still feel sad most days, but I managed to go for two walks.” Reports difficulty concentrating at work and mild insomnia (3–4 hours of sleep per night). Denies suicidal ideation, plan, or intent. Expresses frustration about lack of progress but acknowledges some small improvements.
O – Objective
Client appeared appropriately dressed and oriented ×4. Affect was congruent with mood (depressed, subdued). Speech was normal in rate and tone. Thought processes were logical and goal-directed. No psychomotor agitation or retardation observed. Eye contact intermittent.PHQ-9 administered: score decreased from 18 (moderate-severe) to 14 (moderate) since last session.
A – Assessment
Client continues to meet criteria for moderate major depressive disorder. Mild improvement observed in motivation and activity level. Increased insight into negative thinking patterns. Client is responsive to CBT interventions targeting cognitive distortions. Persistent sleep disturbance and low energy remain areas of concern. Progress appears steady but gradual.
P – Plan
- Continue CBT with focus on identifying and reframing negative automatic thoughts.
- Introduce behavioral activation strategies to increase daily structure and rewarding activities.
- Encourage sleep hygiene techniques (consistent bedtime routine, limit screen time before bed).
- Reassess depression symptoms using PHQ-9 in two weeks.
- Coordinate with primary care provider to rule out medical contributors to fatigue.
- Schedule next session for 10/20/2025.
Watch this video to learn how to save time on therapy notes
Modern EHR/practice management platforms (such as TheraPlatform) assist greatly with documentation by providing HIPAA‑compliant, integrated systems for note entry, storage, scheduling, and billing.
They allow therapists to:
- Use templates (e.g. SOAP, DAP, others) to speed note writing and ensure completeness.
- Link notes to treatment plans, goals, and session history so that therapeutic progress is more easily tracked.
- Securely access and share documents (with clients or other providers, where appropriate) and maintain confidentiality.
Meanwhile, AI‑assisted note tools are emerging which can further help clinicians by:
- Automatically transcribing session audio (if permitted) and highlighting key moments (e.g. emotional shifts, major themes).
- Suggesting draft notes or filling in objective or assessment sections based on observed data, freeing up clinicians’ time.
- Supporting consistency and reducing missing components in notes, which helps from both clinical, legal, and insurance perspectives.
Together, structured SOAP ‑ type notes plus good EHR platforms and smart AI tools support better therapeutic outcomes, more efficient workflows, and stronger accountability.
Improving notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
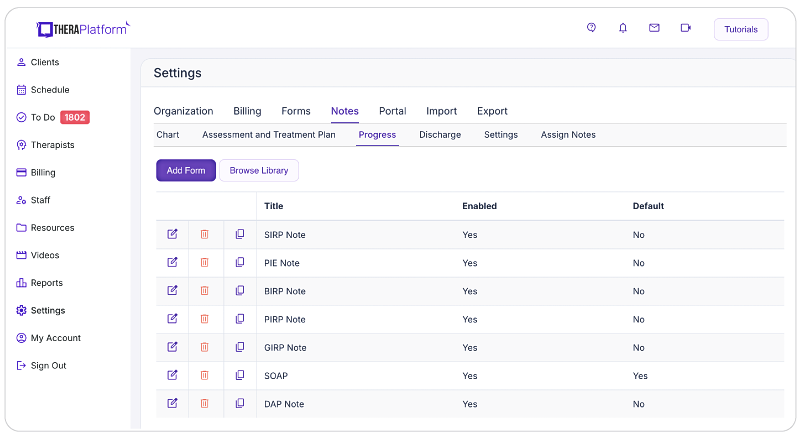
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.

- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.

- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Additional tools and outcome measures to help with data collection and progress monitoring
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
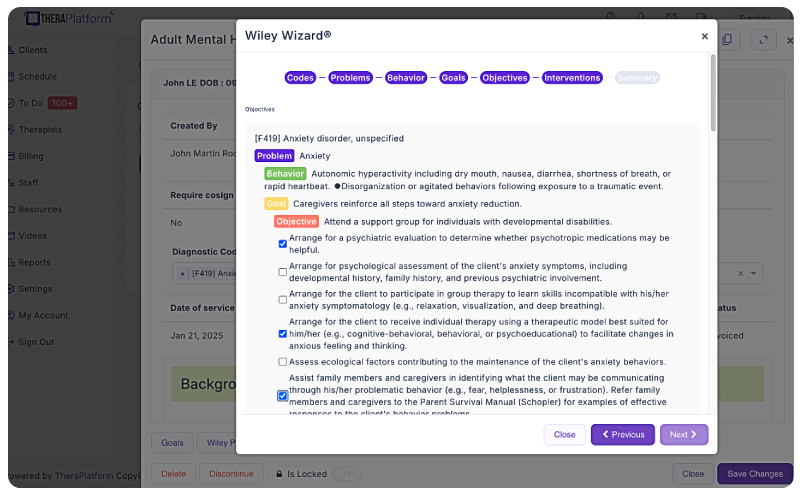
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually.
However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatfrom automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
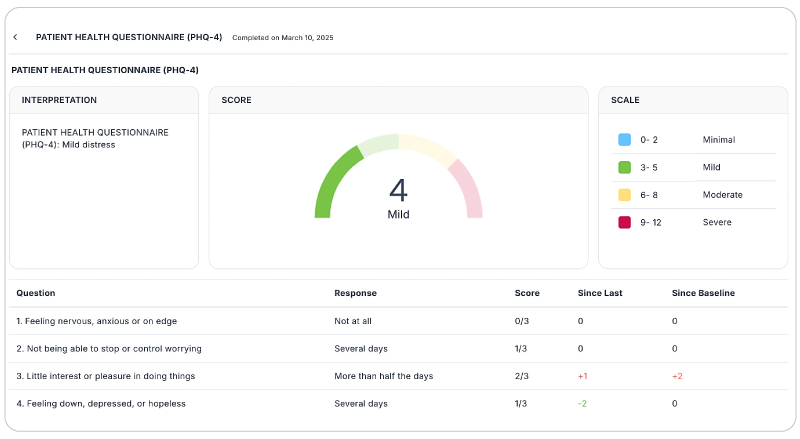
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution with AI-powered note taking that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools
Free video classes
- Free on-demand insurance billing for therapist course
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice
References
Beck, A. T., Steer, R. A., & Brown, G. (1996). Beck Depression Inventory–II (BDI-II) [Database record]. APA PsycTests. https://www.psychiatry.wisc.edu/wp-content/uploads/2019/01/Beck-Depression-Inventory_2017.pdf
EMDR Institute. What is EMDR Therapy? https://www.emdr.com/what-is-emdr
Gautam, M., Tripathi, A., Deshmukh, D., & Gaur, M. (2020). Cognitive behavioral therapy for depression. Indian Journal of Psychiatry, 62(Suppl 2), S223–S229. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_772_19
Halfin A. (2007). Depression: the benefits of early and appropriate treatment. The American Journal of Managed Care, 13(4 Suppl), S92–S97. https://www.ajmc.com/view/nov07-2638ps092-s097
Hamilton M. (1960). A rating scale for depression. Journal of neurology, neurosurgery, and psychiatry, 23(1), 56–62. https://doi.org/10.1136/jnnp.23.1.56
Hill, T., Jiang, Y., Friese, C.R. et al. (2020). Analysis of emergency department visits for all reasons by adults with depression in the United States. BMC Emergency Medicine 20, 51. https://doi.org/10.1186/s12873-020-00347-6
Kroenke, K., Spitzer, R. L., & Williams, J. B. W. (2001). The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. https://www.apa.org/depression-guideline/patient-health-questionnaire.pdf
Johns Hopkins Medicine. Mental health disorder statistics. https://www.hopkinsmedicine.org/health/wellness-and-prevention/mental-health-disorder-statistics
Montgomery, S. A., & Åsberg, M. (1979). A new depression scale designed to be sensitive to change. The British Journal of Psychiatry, 134(4), 382–389. https://www.psychdb.com/_media/mood/madrs.pdf
Osman, A., Bagge, C. L., Gutierrez, P. M., Konick, L. C., Kopper, B. A., & Barrios, F. X. (2001). The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment, 8(4), 443–454. https://doi.org/10.1177/107319110100800409
Posner, K., Brown, G. K., Stanley, B., Brent, D. A., Yershova, K. V., Oquendo, M. A., Currier, G. W., Melvin, G. A., Greenhill, L., Shen, S., & Mann, J. J. (2011). The Columbia-Suicide Severity Rating Scale: Initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American Journal of Psychiatry, 168(12), 1266–1277. https://doi.org/10.1176/appi.ajp.2011.10111704
Radloff, L. S. (1977). The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. https://www.apa.org/depression-guideline/epidemiologic-studies-scale.pdf
Stanley B. & Brown G. (2021). Stanley-Brown Safety Plan. https://suicidesafetyplan.com/wp-content/uploads/2024/12/Stanley-Brown-Safety-Plan-05-02-2024.pdf
FAQs about depression assessments
What is the most commonly used depression screening tool?
The PHQ-9 is the most widely used tool for identifying and tracking depression symptoms in clinical and primary-care settings.
Are self-report depression tests reliable?
Yes, but they rely on client honesty and self-awareness. Clinicians often pair them with interviews or clinician-rated scales for a fuller picture.
How often should depression be reassessed?
Reassessment is typically done at regular intervals or when symptoms change — helping therapists track progress and modify treatment as needed.



