Bipolar disorder ICD 10

Bipolar disorder ICD 10 code is used by healthcare professionals in billing for bipolar disorder, a mental health condition marked by intense psychological highs and lows. Bipolar disorder is a complex journey and affects millions of people worldwide, making it crucial for healthcare professionals to accurately diagnose and document it. In this article, we delve into the realm of bipolar disorder and explore the significance of bipolar disorder ICD 10 codes in understanding and addressing this condition.
Summary
- The ICD-10 code for bipolar disorder is F31, with specific codes like F31.0 for Bipolar I and F31.81 for Bipolar II to differentiate subtypes for accurate diagnosis and billing. Enrolling in an insurance billing course for therapists can help providers enhance their knowledge.
- Evidence-based treatments—such as CBT, IPSRT, Family-Focused Therapy, and medication—play a key role in stabilizing mood and improving quality of life for individuals with bipolar disorder.
- Proper documentation and coding not only support continuity of care but also ensure compliance with insurance and reimbursement requirements.
- Integrated EHR and billing software like TheraPlatform can automate tasks like invoicing, claims submission, and payment tracking, saving providers time and reducing errors.
→ Click here to enroll in our free on-demand Insurance Billing for Therapists video course [Enroll Now]
Overview of bipolar disorder and clinical presentation
Bipolar disorder, previously referred to as manic-depressive illness, is a psychiatric condition characterized by significant mood swings, alternating between episodes of mania and depression. During manic episodes, individuals may experience heightened energy levels, increased impulsivity, and an elevated sense of euphoria. Conversely, depressive episodes bring overwhelming sadness, lethargy, and a pervasive sense of hopelessness.
These mood fluctuations can disrupt various aspects of an individual's life. In manic phases, people may engage in risky behaviors and exhibit impaired judgment, while depressive episodes can make daily tasks challenging, leading to social withdrawal and reduced interest in once-enjoyable activities.
Streamline your insurance billing with One EHR
- Claim batching
- Auto claims
- Automated EOB & ERA
- Real-time claim validation
- Real-time claim tracking
- Aging and other reports

The oscillation between these states not only affects the individual but also strains relationships within their social and familial circles. The unpredictable nature of mood shifts can make it challenging for friends and family to understand and cope with the changes in behavior. Employment and educational pursuits may also be hindered due to fluctuations in energy levels and focus.
Important to note: The overall well-being of individuals with bipolar disorder is closely tied to the management of these mood swings. The condition can be isolating, intensifying feelings of loneliness and frustration. Recognizing the clinical presentation of bipolar disorder is crucial for healthcare practitioners.
Understanding how this disorder manifests allows healthcare professionals to provide timely and effective intervention. Early detection and intervention can significantly improve outcomes, enabling individuals with bipolar disorder to lead more stable lives. By comprehending the subtleties of the clinical presentation, healthcare practitioners can tailor treatment plans to address the unique needs of each individual, promoting resilience and minimizing the impact of this challenging mental health condition on their daily lives.
What is the ICD-10 code for bipolar disorder?
The International Classification of Diseases, 10th Edition (ICD-10), is a globally recognized coding system that categorizes various health conditions, facilitating accurate diagnosis and streamlined communication within the healthcare community. This system does a wonderful job ensuring uniformity in medical documentation and billing.
Bipolar disorder ICD 10 code: F31
Within the extensive ICD-10 catalog, the bipolar disorder ICD code is F31. This alphanumeric code serves as a specific identifier for healthcare providers, insurance companies, and researchers. The utilization of ICD-10 codes enhances the precision of medical records, ensuring that bipolar disorder is accurately captured in a standardized format.
What is the difference between bipolar disorder ICD 10 codes for bipolar I and bipolar II?
Bipolar I Disorder disorder (F31.0)
Bipolar I Disorder is characterized by the presence of at least one manic episode, which may be accompanied by hypomanic or major depressive episodes. Understanding the specific bipolar disorder ICD 10 code (F31.0) for Bipolar I Disorder aids in distinguishing it from other subtypes.
Bipolar II Disorder (F31.81)
Bipolar II Disorder is marked by recurrent depressive episodes and hypomanic episodes, but not full-blown manic episodes. The bipolar disorder ICD 10 code (F31.81) for Bipolar II facilitates accurate identification and differentiation within the coding system. Because treatment for Bipolar 1 and Bipolar II may vary significantly, differentiating the two is necessary.
Other bipolar disorder ICD 10 code subtypes and specifiers
Cyclothymic Disorder (F34.0)
Cyclothymic Disorder is a milder form of bipolar disorder, characterized by numerous periods of hypomanic and depressive symptoms. The bipolar disorder ICD 10 code (F34.0) for Cyclothymic Disorder ensures proper documentation of this subtype.
Understanding these subtypes and their corresponding bipolar disorder ICD 10 codes is imperative for healthcare professionals aiming to capture the nuanced presentations of bipolar disorder accurately.
Watch this video to learn common insurance billing struggles and solutions
→ Start My Free Trial
→ Start My Free Trial
Evidence-based therapeutic approaches for bipolar disorder
Incorporating these evidence-based therapeutic approaches into the treatment plan offers a holistic and personalized strategy for managing bipolar disorder, addressing not only the symptoms but also the underlying factors that contribute to the disorder's complexity.
Cognitive-Behavioral Therapy (CBT):
Cognitive-Behavioral Therapy (CBT) has emerged as a promising therapeutic approach for individuals grappling with bipolar disorder. This psychotherapeutic intervention focuses on identifying and modifying dysfunctional thought patterns and behaviors. In the context of bipolar disorder, CBT aids individuals in recognizing triggers and early warning signs of mood episodes. By fostering self-awareness and developing coping strategies, CBT empowers individuals to navigate the challenges posed by both manic and depressive phases. Moreover, CBT is particularly beneficial in preventing the recurrence of mood episodes, contributing to long-term stability.
Interpersonal and Social Rhythm Therapy (IPSRT)
Interpersonal and Social Rhythm Therapy (IPSRT) is a specialized form of psychotherapy designed to address the interplay between interpersonal relationships and the regulation of daily routines. For individuals with bipolar disorder, disruptions in social rhythms and sleep-wake cycles can trigger mood episodes. IPSRT helps individuals establish regular routines and enhance interpersonal skills, thereby promoting stability and reducing the risk of relapse. By addressing the social and environmental factors that contribute to mood disturbances, IPSRT provides a comprehensive approach to managing bipolar disorder.
Family-Focused Therapy (FFT)
Recognizing the impact of bipolar disorder on familial dynamics, Family-Focused Therapy (FFT) becomes a crucial element in comprehensive treatment. This approach involves educating family members about the nature of bipolar disorder, enhancing communication skills, and fostering a supportive environment. FFT is instrumental in reducing family-related stressors that may exacerbate the condition. By involving family members in the therapeutic process, FFT not only contributes to the well-being of the individual but also strengthens the overall family unit.
Medication
Pharmacotherapy is a cornerstone in the management of bipolar disorder. Mood stabilizers, antipsychotics, and antidepressants are commonly prescribed to help regulate mood swings. Lithium, in particular, is a widely used mood stabilizer that has shown efficacy in preventing both manic and depressive episodes. The choice of medication is tailored to the specific needs and response of each individual. Regular monitoring and adjustment of medication, under the guidance of a psychiatrist, are essential components of the treatment plan.
Psychoeducation
Psychoeducation plays a pivotal role in empowering individuals with bipolar disorder to actively participate in their treatment. This educational approach provides comprehensive information about the nature of the disorder, its potential triggers, and effective coping strategies. Psychoeducation not only enhances the individual's understanding of their condition but also promotes adherence to treatment plans. By fostering a sense of control and self-efficacy, psychoeducation contributes to the overall management and well-being of individuals living with bipolar disorder.
Practice Management + EHR + Telehealth
Mange more in less time in your practice with TheraPlatform

Family and support system involvement for bipolar disorder
Navigating bipolar disorder is not a solitary journey, and the involvement of family and support systems plays a pivotal role in the overall well-being of individuals facing this mental health challenge. Family and support system involvement can provide a crucial safety net, offering understanding, encouragement, and assistance in managing the complexities associated with bipolar disorder. Establishing open lines of communication, fostering empathy, and educating family members about the disorder contribute to a supportive environment that aids individuals in their recovery journey.
Co-occurring disorders and dual diagnosis
Substance use disorders in bipolar clients
The intricate relationship between bipolar disorder and substance use disorders adds an additional layer of complexity to treatment. Individuals with bipolar disorder are at an increased risk of developing substance use disorders, as self-medication may become a coping mechanism. Addressing substance use disorders concurrently with bipolar disorder is imperative for successful outcomes. Tailored interventions, including psychotherapy and support groups, are essential components of a comprehensive treatment plan.
Addressing anxiety, ADHD, and other comorbidities
Bipolar disorder often coexists with other mental health conditions, such as anxiety and attention-deficit/hyperactivity disorder (ADHD). Recognizing and addressing these comorbidities is crucial for accurate diagnosis and effective treatment. An integrated approach that considers the interplay of various conditions ensures a holistic and personalized intervention strategy. Psychoeducation, medication management, and targeted therapies become essential in addressing the diverse needs of individuals with bipolar disorder and comorbidities.
Integrated treatment approaches
Integrating treatment modalities for co-occurring disorders is a cornerstone of comprehensive mental health care. Collaborative efforts between mental health professionals specializing in bipolar disorder, substance use disorders, anxiety, ADHD, and other comorbidities result in a more cohesive and effective treatment plan. Coordinated care ensures that individuals receive tailored interventions addressing the unique challenges posed by both bipolar disorder and co-occurring conditions.
Documentation and bipolar disorders ICD 10 coding
Accurate recording of bipolar disorder diagnosis
Accurate and thorough documentation of bipolar disorder diagnosis is essential for providing quality care and facilitating effective communication among healthcare professionals. The bipolar disorder ICD 10 code F31 serves as a precise identifier, ensuring standardized representation of bipolar disorder in medical records. Clear and detailed documentation enhances continuity of care, allowing for a comprehensive understanding of an individual's treatment history and progress.
Compliance with insurance and billing requirements
The accurate application of bipolar disorder ICD 10 codes not only aids in clinical communication but also ensures compliance with insurance and billing requirements. Proper coding facilitates streamlined reimbursement processes, reducing administrative burdens for healthcare providers and enhancing the financial sustainability of mental health services. Compliance with coding standards is paramount in navigating the intricacies of the healthcare reimbursement landscape.
Importance of thorough clinical notes
Thorough clinical notes are the backbone of effective mental health care. Beyond bipolar disorder ICD 10 codes, detailed clinical documentation captures the nuances of an individual's response to treatment, fluctuations in symptoms, and any adjustments made to the care plan. These notes contribute to informed decision-making, collaboration among healthcare professionals, and, importantly, serve as a legal record of the care provided. Investing time in comprehensive clinical notes ensures a holistic and patient-centered approach to managing bipolar disorder.
Encouraging hope and recovery in bipolar clients
Despite the challenges of bipolar disorder, it's crucial to emphasize that things can improve. By using effective therapies, including loved ones, and addressing other issues that might come up, people with bipolar disorder can work towards feeling more stable and better overall. Encouraging hope is a powerful tool, helping individuals face and overcome the hurdles on their way to recovery.
Commitment to ongoing professional development in bipolar care
For those in the healthcare field, our dedication doesn't end here. We commit to always learning and growing in how we care for all patients. Keeping up with new research and better ways to treat bipolar disorder ensures that we offer the best support possible. This commitment ensures that we stay updated and provide the most effective care as the field of mental health progresses.
By working together, understanding the disorder, and adapting to new tools, we can provide support that gives hope, aids recovery, and keeps us at the forefront of effective bipolar disorder care.
In summary, we've covered important aspects of dealing with bipolar disorder; from recognizing its signs and using the right codes for it to trying out helpful therapies and involving family, these takeaways highlight the need for a thorough and team-based approach.
How EHR and practice management software can save you time with insurance billing for therapists
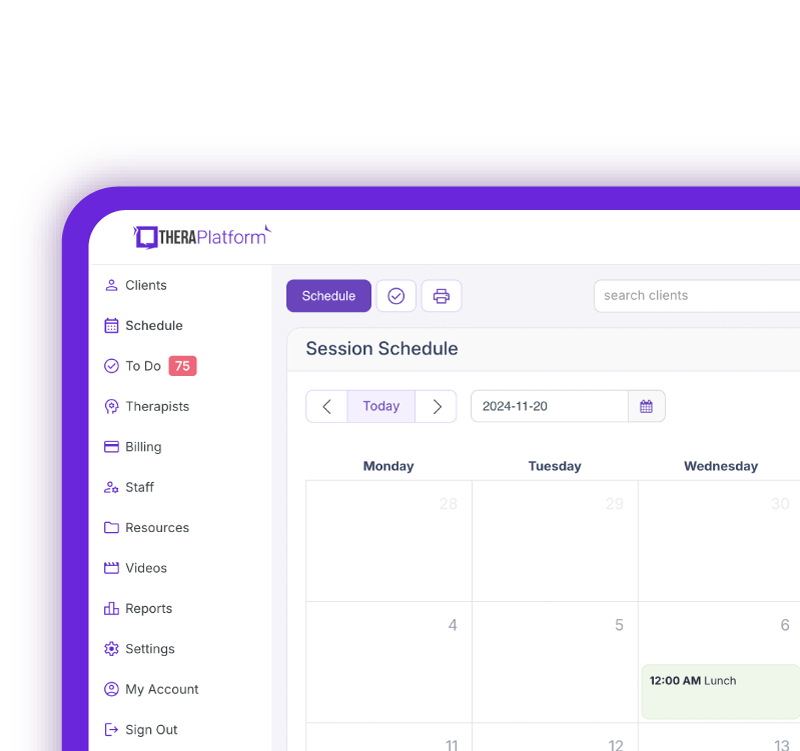
EHR with integrated billing software and a clearing house, such as TheraPlatform, offers significant advantages in creating an efficient insurance billing process. The key is minimizing the amount of time dedicated to developing, sending, and tracking medical claims through features such as automation and batching.
What are automation and batching?
- Automation refers to setting up software to perform tasks with limited human interaction.
- Batching or performing administrative tasks in blocks of time at once allows you to perform a task from a single entry point with less clicking.
Which billing and medical claim tasks can be automated and batched through billing software?
- Invoices: Create multiple invoices for multiple clients with a click or two of a button or set up auto-invoice creation, and the software will automatically create invoices for you at the preferred time. You can even have the system automatically send invoices to your clients.
- Credit card processing: Charge multiple clients with a click of a button or set up auto credit card billing, and the billing software will automatically charge the card (easier than swiping!)
- Email payment reminders: Never manually send another reminder email for payment again, or skip this altogether by enabling auto credit card charges.
- Automated claim creation and submission: Batch multiple claims with one button click or turn auto claim creation and submission on.
- Live claim validation: The system reviews each claim to catch any human errors before submission, saving you time and reducing rejected claims.
- Automated payment posting: Streamline posting procedures for paid medical claims with ERA. When insurance offers ERA, all their payments will post automatically on TheraPlatform's EHR.
- Tracking: Track payment and profits, including aging invoices, overdue invoices, transactions, billed services, service providers.
Utilizing billing software integrated with an EHR and practice management software can make storing and sharing billing and insurance easy and save providers time when it comes to insurance billing for therapists.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax
Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tool
- Behavioral Health tools