SOAP Notes for Speech Therapy: The Ultimate Guide

SOAP Notes. Whether you’re a new grad or seasoned clinician, perfecting your treatment note is a crucial part of any speech therapist’s practice.
Summary
- Speech therapy SOAP notes should be clear, consistent, and concise are characteristics that help ensure accurate documentation that is easy to understand for therapists, caregivers, and insurance providers. Download my free SOAP notes template.
- Each speech therapy SOAP Note has four sections: Subjective (observations), Objective (measurable data), Assessment (interpretation of progress), and Plan (next steps), ensuring a comprehensive record of each session.
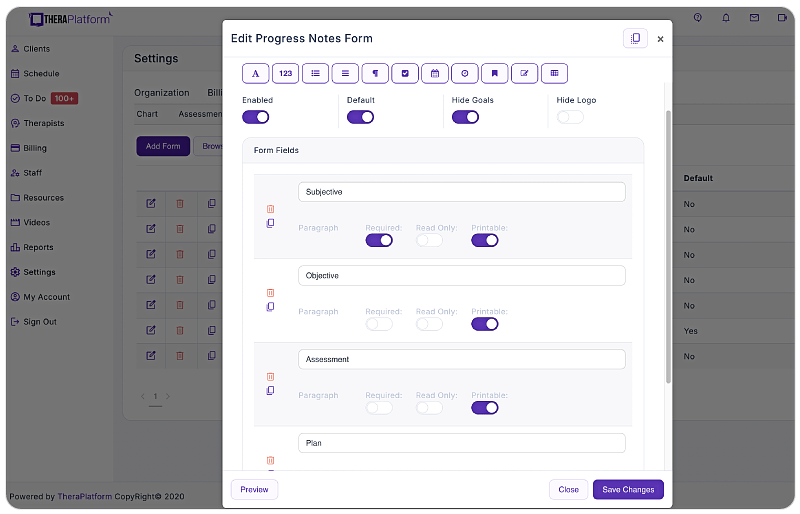
- Using an electronic health record (EHR) system like TheraPlatform with built-in templates and automation can save speech therapists time and improve the accuracy of their documentation.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Speech therapy SOAP notes document important data and paint a picture of how the client participated in a session. That’s not always easy. A speech-language pathologist’s (also known as “SLP”) schedule is often filled with back-to-back clients throughout the day.
Having a clear understanding of what SLP SOAP notes are, and how to write one both thoroughly and efficiently can be a huge help to SLPs. This helps them feel confident that they documented the necessary information for insurance and legal purposes while not falling behind on paperwork or getting backed up on time.
What is an SLP SOAP Note?
SLP SOAP notes are a written document that reports on what was done in a therapy session. It should be written the same day as the session occurred. This timely documentation ensures accurate and up-to-date documentation is completed. Additionally, SLP SOAP notes must be completed the same day as the service because they are attached to charges for the session.
The SOAP note can be written after the session. Or, if the SLP uses an easily accessible, concise SOAP note template, the note can be written during the last few minutes of the session itself. TheraPlatform offers a built-in SLP SOAP note template that is clear, consistent, and concise. This allows SLPs to complete the soap note template during the session, making documentation with back-to-back therapy sessions a breeze.
Practice Management + EHR + Telehealth
Mange more in less time in your practice with TheraPlatform

.
What’s in a SOAP note?
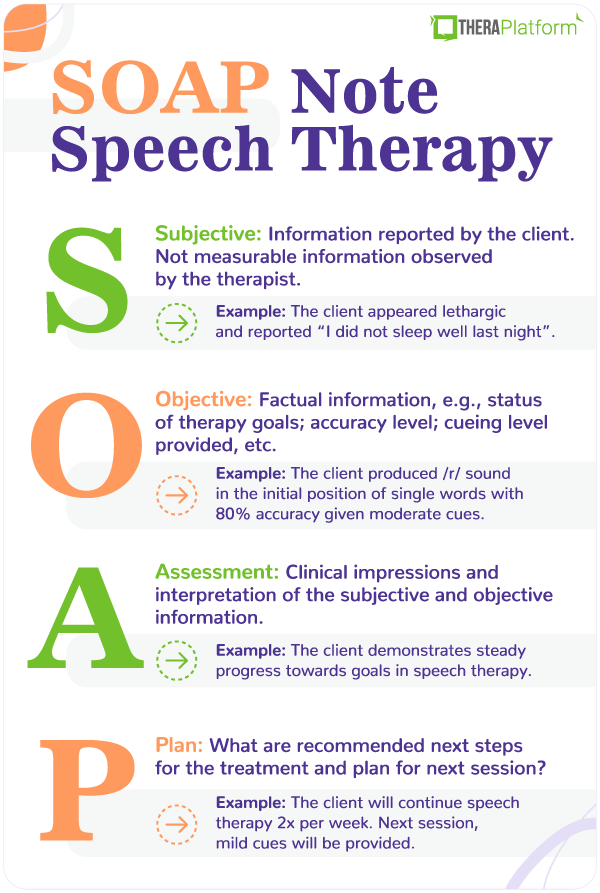
SOAP stands for the 4 sections that make up the therapy note: Subjective, Objective, Assessment and Plan.
It may be shared with the client and/or his or her caregiver, as well as insurance companies. Here’s a closer look at what makes up a SOAP note, and the do’s and don’ts to keep in mind when writing each section along with a SOAP note example.
Subjective
This is a brief statement that describes a client’s state from the therapist’s point of view.
The information in this section isn’t measurable, and can be gathered both from the therapist’s observations and any information given by the caregiver who accompanies the client to the session.
What questions can you answer in the subjective section of your speech therapy SOAP note?
- Behavior (e.g., frequent refusals, cooperative, engaged, attentive)
- Medical status (e.g., recent illness)
- Current state (e.g., alert, lethargic/tired)
Do’s of writing the subjective section
- Keep it brief (about 1-3 sentences)
- Back up statements with supporting information such as quotes. (e.g, Mother reported “he woke up early and is tired today.”)
- Paint a clear picture of how the client participated in the session
Don’ts of writing the subjective section
- Make it too lengthy
- Include information that is irrelevant or unnecessary
Speech therapy SOAP note examples: Subjective section
- Johnny appeared alert, and transitioned into the therapy room without difficulty. He was engaged and participated in all therapeutic activities that were presented.
- Alice became upset and clung to her mother upon entering the therapy room. She frequently put her head down and refused to participate in tasks.
- Cayden appeared lethargic and his mother reported, “he didn’t sleep well last night”. He was engaged and interactive when provided with positive reinforcement and praise.
Objective
The objective section is all about stating the facts. The information an SLP writes here must be measurable or quantitative. This usually includes reporting on therapy goals and stating the data that the client achieved for each goal targeted during the session.
When thinking of this section, think percentages, numbers, accuracy level, and scores.
Here, the speech-language pathologist will also state whether each therapy goal was targeted, not targeted, met, not met, or progressing.
What questions can you answer in the objective section of your SOAP note?
- Short term/current therapy goals
- Data reporting the client’s performance on each goal (percentage accuracy or number of times the client performed the targeted task)
- Cueing level provided for each goal (for example, maximum, moderate, minimal cues, or independently)
- If the goal was met or not met for that session
- Number of consecutive sessions in which each goal achieved has been met (e.g., 1 out of 3 consecutive sessions)
Do’s of writing the objective section
- Be clear and concise
- Include measurable data
- Report on the client’s performance
- Address each current therapy goal (if not addressed, mark as “not targeted”)
Don’ts of writing the objective section
- Don’t include lengthy descriptions of the therapy activities.
- Don’t write subjective information that cannot be quantified
Speech therapy SOAP note example: Objective section
- Johnny produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal Met for 2 out of 3 consecutive sessions)
- Olivia identified common objects in 7 out of 10 opportunities given minimal cues. (Goal Progressing/Not Met)
- Allison used irregular past tense verbs at the sentence level with 50% accuracy independently. (Goal progressing/not met)
Assessment
In the Assessment section of a SOAP note, a speech-language pathologist analyzes and interprets the information documented within the first two sections (the Subjective and Objective sections).
What questions can you answer in the Assessment section of your SOAP note?
- Is the client making progress towards goals overall?
- Are there any barriers to progress? For example, medical status, attendance, or the client’s behavior?
Do’s of writing the assessment section
- Note client’s response to receiving speech therapy (e.g., positive)
- Compare client’s performance to that of previous sessions
Don’ts of writing the assessment section
- Restate information already reported on in the subjective or objective sections
Speech therapy SOAP note example: Assessment
- Ethan continues to demonstrate steady progress towards goals in speech therapy.
- Logan’s behavior is impeding his progress towards goals in speech therapy.
- Mila’s production of the /th/ sound improved by 15% compared to her previous session.
Plan
In this final section of the SOAP note, the therapist writes the recommended next steps for the client’s treatment.
These questions should be answered in the plan section of your SOAP note:
- Is continued treatment recommended?
- Should the client be discharged from speech therapy services?
- Are there any recommended changes to the treatment plan? If so, why? (e.g., a reduction in therapy from 2 times per week to 1 time per week due to the client’s progress towards therapy goals).
- Are there any other therapy services recommended going forward for this client? For example, “It is recommended that the client receive a formal audiological evaluation to rule out hearing difficulties”.
When writing the plan section of your speech therapy SOAP note, do:
State any recommended changes for the next therapy session. For example, “The next therapy session will focus on recording Alex’s speech and encouraging him to monitor it for articulation errors”.
Don’t
- Forget to back up your recommendations.
SOAP note example(s): Plan
- Client is approaching goal status for /r/ articulation. In the next session, /r/ words in the medical section will be introduced.
- Continue with current plan and evaluate each week
Watch this video to learn how to save time on therapy notes
→ Start My Free Trial
→ Start My Free Trial
How to write a SOAP note
One part of writing a SOAP note is knowing what information to include. The other part is knowing how to document this information. Remember, clear, consistent, and concise are words an SLP should keep in mind when writing a SOAP note.
The benefits of writing session notes (SLP SOAP notes) in this way include:
- The therapist can easily refer to SLP SOAP notes from the previous session to compare progress.
- Parents and caregivers are able to better understand speech therapy goals and how the client is performing in sessions.
- Other professionals working with the client (e.g., teachers, occupational therapists, and ABA therapists) can view his or her therapy plan for speech.
- Required documentation can be more easily located by insurance providers and reviewers for reimbursement purposes.
- Now, let’s look at what those characteristics mean, and how SLPs can apply them to their daily notes.
Clear SLP SOAP notes samples
What does this mean for your SLP SOAP note?
You want to write it in a way that readers can easily understand the information. Some clinical terminology will be used. However, the note should describe the client’s performance during a session in a way that others who may not have a clinical background can still understand.
Let’s take a look at a clear SLP SOAP note example vs. a SOAP note example that is less clear.
Clear
Objective: Client produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal met for 2 out of 3 consecutive sessions)
Not clear
Objective: Client was able to accurately produce /r/ while reading a story about rabbits. He had more difficulty producing the final /r/ than the medial /r/, and was stimulable for corrections with verbal and tactile cueing. Client was excited that he will have a baseball game today. He liked the book but started crying during the game.
In the second, less clear SOAP note example, the longer description of the client’s performance is unclear to the reader. The specific goal targeted is not easy to determine. The reader is unsure of what word position the goal is for the /r/ sound to be produced.
The objective section in the less clear SOAP note example also leaves the reader questioning at what level the sound is being targeted (ex: single words or sentences). The second SOAP note example also includes extraneous information that is not clinically relevant. Professionally worded statements about the client’s state (ex: engaged, uncooperative) should be included in the “Subjective” part of the SOAP note.
The first, clear SOAP note example on the other hand, would be easier for the audience to understand. Only the most important clinical information is included. The objective section here clearly states the target sound, word position, level of hierarchy, and percentage that provides an objective report on the client’s performance.
Keep the purpose in mind
Another reason speech pathologists should keep their SLP SOAP notes clear? To fulfill the purpose of the note. The purpose of SLP SOAP notes is to clearly and accurately document a client’s diagnosis, the treatment being provided, and his or her progress.
Free Resources for Therapists
Click below and help yourself to peer-created resources:
Consistent SLP SOAP notes
SLP SOAP notes should appear consistent over time. If a client is seen for ongoing therapy at a given frequency (ex: weekly or monthly), the format of the SLP SOAP notes should look standardized. The specific clinical information such as the therapy goals, client’s state, and progress, will of course differ from one session to the next.
Using a SOAP note template makes it easy for an SLP’s SOAP notes to appear consistent overall. For one thing, it is simple for the SLP to input information about the session into a SOAP note template. Secondly, when using a SOAP note template, others can track and compare documentation over time. This can be important for the reader (such as an insurance reviewer) to easily compare documentation over a span of time to see if the client is demonstrating overall progress by receiving speech therapy.
Consistency with SOAP note templates means information is documented in the same place and format from one session to the next.
Concise SLP SOAP notes
Documenting only the clinically relevant, most pertinent information about a session provides the following benefits:
- It is easier for the reader to locate information.
- It appears professional.
- Concise SLP SOAP notes help ensure only the most important clinical information is included.
How long should SLP SOAP notes be?
SLP SOAP notes should contain approximately 1 small paragraph per section.
Some sections may have more information than others.
- Subjective: This section will likely contain 1-2 sentences describing the client’s state. For example, “Hannah was alert and engaged. She participated in all activities presented.” Or, “Owen appeared tired and required cues to participate in the therapy session. Mother reported he has been sick this week.”
- Objective: This will likely be the longest section of an SLP’s SOAP note. Since this is where the goals will be listed and reported on, the length will depend on how many current goals are being targeted in therapy.
- Assessment: The assessment section will likely contain approximately 4 to 5 statements. If the SLP uses a SOAP note template, this could be completed by marking checkboxes of statements that apply to the client’s current status in therapy.
- Plan: This is a short statement or two that will likely be bulleted and includes plans for future sessions.
For example, the SLP may only need to check boxes of statements on a SOAP note template that provide statements such as, “Recommend continue therapy per plan of care”, or “Client continues to demonstrate improvements in Speech Therapy.”
The entire note itself should not exceed 1 to 2 pages. Remember, to serve its purpose to provide parents, other professionals, and insurance reviewers necessary clinical information, the note should be succinct.
SOAP note example: Entire note
Using an SLP SOAP note template makes writing notes fast, efficient, and comprehensive.
Here’s a complete SLP SOAP note example:
S: Johnny appeared alert, and transitioned into the therapy room without difficulty. He was engaged and participated in all therapeutic activities that were presented.
O: Client produced the /r/ sound in the initial position of single words with 80% accuracy given moderate cues. (Goal Met for 2 out of 3 consecutive sessions.) Client used personal pronouns accurately in 6/10 opportunities given minimal cues (Progressing/Goal not met.)
A: Johnny continues to demonstrate steady progress towards goals in speech therapy.
P: It is recommended Johnny continue with the current treatment plan of 2 times per week for 30 minutes per session, for an estimated duration of 180 days.
Download My Free Therapy SOAP Notes Template
Improving notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and efax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
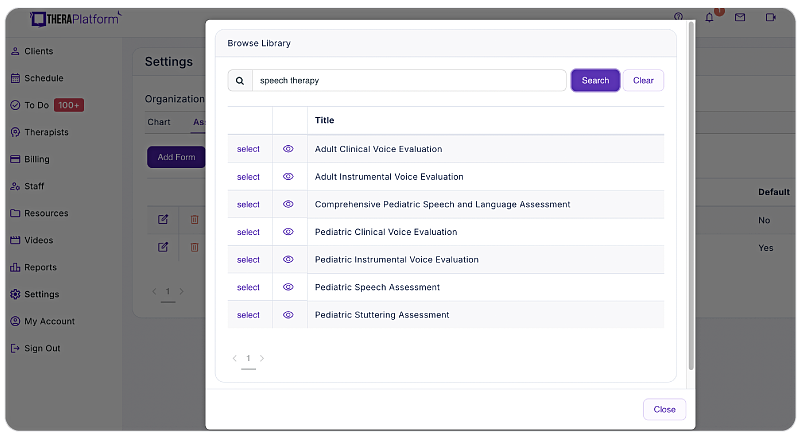
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.
- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.
- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers efax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
TheraPlatform is an all-in-one EHR, practice management, and teletherapy software built for therapists to help them save time on admin tasks. It offers a 30-day risk-free trial with no credit card required and supports different industries and sizes of practices, including speech-language pathologists in group and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools