Occupational therapy SOAP note

Occupational therapy SOAP note, an overview of SOAP notes, questions to ask when writing each section, the do’s and don’ts of writing soap notes, the benefits of using SOAP notes in occupational therapy, and an example of an occupational therapy SOAP note will be covered in this post.
Summary
- The SOAP format - Subjective, Objective, Assessment, Plan - ensures that occupational therapists document all essential components of a therapy session, from client reports to intervention planning, making them ideal for clinical reasoning and interdisciplinary communication. Download my free SOAP notes template.
- Key do’s and don’ts include documenting in the correct order, avoiding copy-paste habits, including quantitative data, and justifying medical necessity to support reimbursement and audit preparedness.
- These notes serve not only as legal and clinical documentation but also help with intervention planning, tracking client progress, and writing discharge summaries and progress reports.
- Platforms like TheraPlatform simplify the creation, customization, storage, and secure sharing of SOAP notes through features like templates, note duplication, HIPAA-compliant storage, e-signatures, and integrated e-faxing.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

How to write an occupational therapy SOAP note
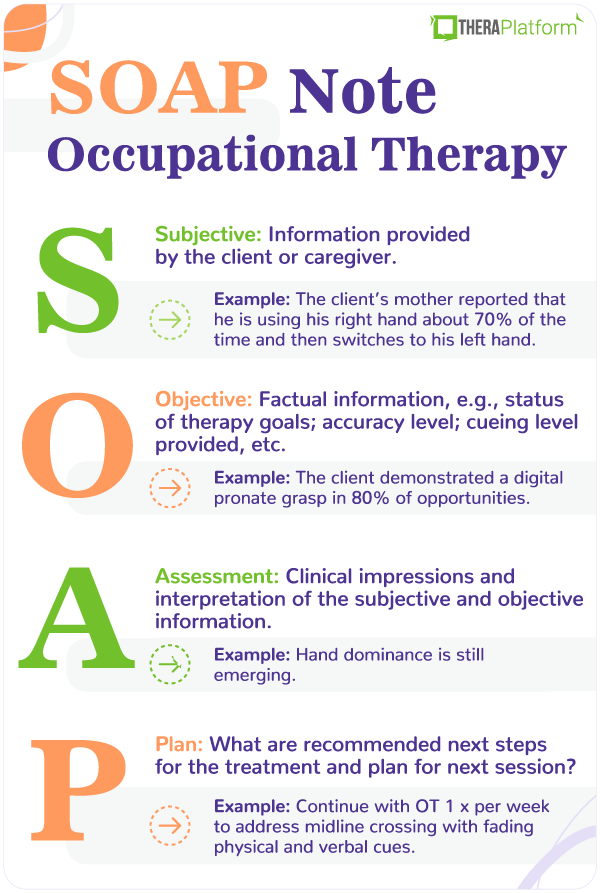
The SOAP note method of documentation can be an excellent fit for the occupational therapy profession. Why does it work well for OTs? We are always looking at the big picture. SOAP is an acronym that stands for subjective; objective; assessment; plan. These are all important components of occupational therapy intervention and should be appropriately documented. Using a SOAP note format will help ensure that no essential element of therapy is left undocumented.
Here are the different components and questions to ask yourself.
S: Subjective
- What is the client reporting?
- What are the client’s parents or caregivers reporting?
- Is the client reporting pain?
- Are they complaining of fatigue?
O: Objective
- What level of assistance did the client need?
- How many verbal and physical prompts were provided?
- What did you observe?
- How did you grade the activity or modify the environment?
- In what percentage of trials was the client successful?
- What is progress is the client currently making on their goals?
A: Assessment
- After examining the subjective and objective data, what does this mean about your client’s progress?
- Why did you select a certain intervention activity?
- Have there been any significant changes in functioning?
P: Plan
- Should the treatment plan be changed? How?
- Does a new referral need to be made?
- Are any accommodations or modifications recommended?
The Do’s and Don’ts of occupational therapy SOAP Notes
Remember, the SOAP acronym isn’t completely exclusive when it comes to what you need in your documentation.
Do’s
- Do remember to include the patient’s name, date of birth, date and time of the service, as well as your own credentials and signature.
- Do use the SOAP note format in order. It is commonly recognized by a variety of health professionals. Following the standard order can help your interdisciplinary team find the information that they need, fast.
- Do include justification that the services are medically necessary. This is essential for reimbursement by third-party payers.
- Accurately document your client’s progress by ensuring that each SOAP note is unique to that therapy session.
Don’ts
- Don’t put your observations or assessment into the subjective section. The subjective category is a way to capture your client’s voice, perspectives, and goals.
- Don’t neglect to provide quantitative data. This will help you select future interventions and keep track of patient progress.
- Don’t copy and paste. While some of the information may look similar from session to session, it is disadvantageous to leave out specific data from a given session.
Practice Management + EHR + Telehealth
Mange more in less time in your practice with TheraPlatform

Benefits of occupational therapy SOAP notes
- SOAP notes can be beneficial in the event of an insurance audit. The narrative format helps capture a unique session and each SOAP note should be distinct. The subjective data especially helps to verify that the therapy session occurred.
- A complete SOAP note should clarify the skilled processes of occupational therapy. In addition to adding credibility that the session happened, in the event of an insurance audit auditors will be looking for skilled intervention. This will be covered in your assessment section.
- Managing a large caseload? SOAP notes make a great tool for intervention planning. When planning an upcoming session you will look at your previous SOAP note to determine your plan. At this point you will have already used your clinical reasoning to make an assessment and plan for the upcoming session.
- SOAP notes are helpful for writing progress and discharge notes. With the narrative form of a SOAP note, you can easily access quantitative and qualitative data that relate directly back to functioning.
- SOAP notes are a commonly used format among health professionals and are meant to be short and succinct. This can help you or another healthcare provider quickly and easily find the information that is needed.
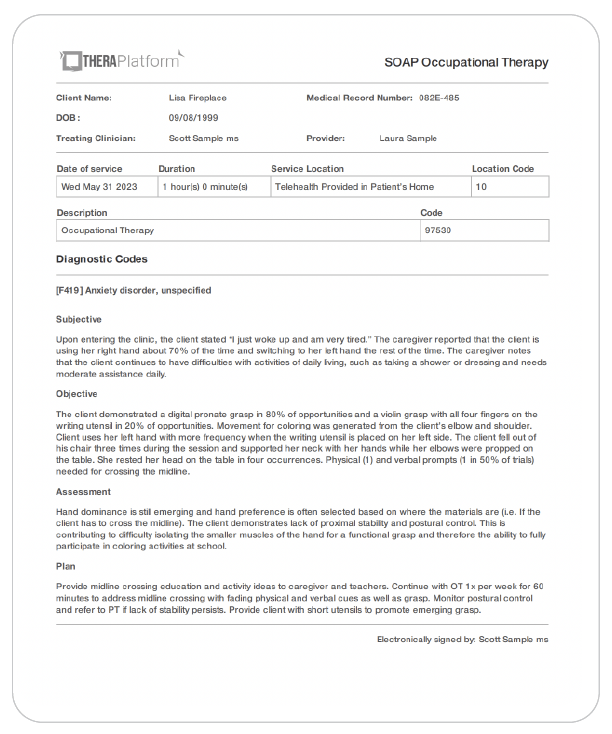
Occupational Therapy SOAP note example
Here is an example of occupational therapy SOAP note.
This client has two goals. Briefly: Crossing the midline while participating in functional activities at school and using a functional grasp with a variety of writing utensils.
S: Upon entering the clinic, the client stated “I just woke up and am very tired.” The caregiver reported that the client is using his right hand about 70% of the time and switching to his left hand the rest of the time.
O: The client demonstrated a digital pronate grasp in 80% of opportunities and a violin grasp with all four fingers on the writing utensil in 20% of opportunities. Movement for coloring was generated from the client’s elbow and shoulder. Client uses his left hand with more frequency when the writing utensil is placed on his left side. The client fell out of his chair three times during the session and supported his neck with his hands while his elbows were propped on the table. He rested his head on the table in four occurrences. Physical (1) and verbal prompts (1 in 50% of trials) needed for crossing the midline.
A: Hand dominance is still emerging and hand preference is often selected based on where the materials are (i.e. If the client has to cross the midline). The client demonstrates lack of proximal stability and postural control. This is contributing to difficulty isolating the smaller muscles of the hand for a functional grasp and therefore the ability to fully participate in coloring activities at school.
P: Provide midline crossing education and activity ideas to the caregiver and teachers. Continue with OT 1x per week for 60 minutes to address midline crossing with fading physical and verbal cues as well as grasp. Monitor postural control and refer to PT if lack of stability persists. Provide the client with short utensils to promote emerging grasp.
How can EMR software can help with occupational therapy SOAP notes?
EMR software, such as TheraPlatform, offers significant advantages in creating efficient, adaptable, and precise SOAP (Subjective, Objective, Assessment, and Plan) notes for occupational therapists. The key is minimizing the amount of time dedicated to creating, storing/managing and sharing notes through the use of intuitive features.
How to streamline occupational therapy SOAP Notes process
The process around SOAP notes typically involves three steps including creation, storage/access and sharing. An EMR like TheraPlatform can minimize the amount of busywork associated with these steps. Let’s take a look at how TheraPlatform’s features helps streamline the SOAP notes process.
SOAP notes creation
Saving time on creating SOAP notes for occupational therapy can be done in three ways.
- Using a template library: TheraPlatform's EMR provides built-in note templates, including SOAP notes, ensuring occupational therapists maintain consistency and conciseness in their documentation. These templates follow a standardized format, facilitating easy review. You can see an example of TheraPlatform’s built-in therapy note template in the screenshot below.
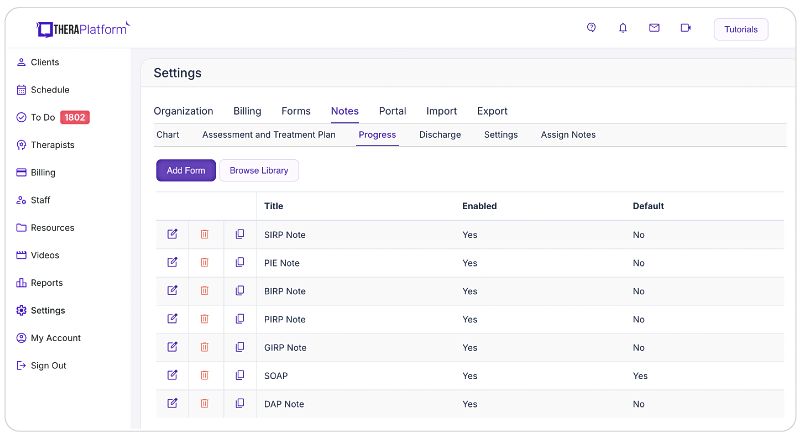
- Customizable note templates: While templates are a great foundation, TheraPlatform's EMR features a flexible note template builder, empowering occupational therapists to customize SOAP note templates according to their preferred documentation style. Whether you prefer the traditional SOAP format, a single narrative field, or the inclusion of checkboxes, the template builder offers versatility and efficiency without the need to completely modify an existing template.
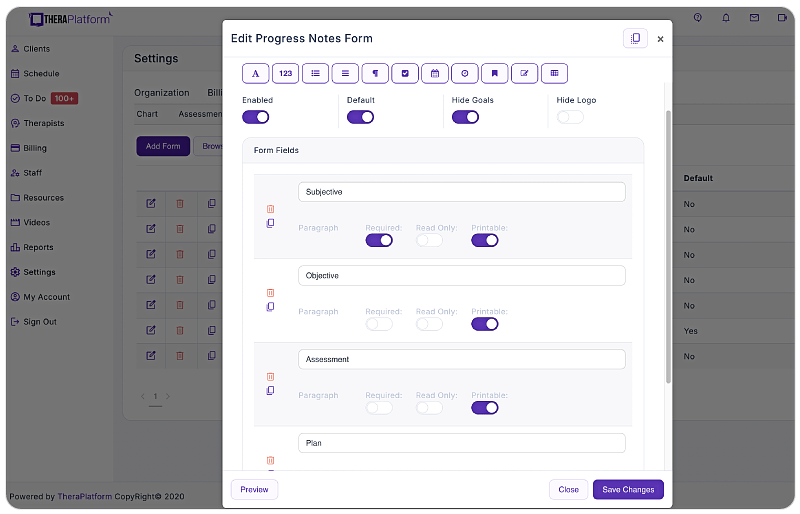
- Duplication: TheraPlatform's EMR enables therapists to save time and maintain consistency by copying notes from previous sessions. This feature simplifies the documentation of recurring information or progress updates, allowing therapists to easily edit and expand upon the copied notes as necessary. No more writing the same information from scratch each and every time.
Occupational therapy SOAP notes and access
- Once SOAP notes are written, they need to be organized in a way that is secure and accessible for the therapists. Oftentimes, manual methods provide more obstacles than efficiency. An EMR can help.
Storage
- HIPAA-Compliant and Secure Storage: Occupational therapy notes contain sensitive client information, necessitating secure and HIPAA-compliant storage. TheraPlatform's EMR ensures adherence to HIPAA regulations, employing robust bank-level security measures to safeguard client data. Additionally, TheraPlatform provides signed Business Associate Agreements (BAAs) for further protection of Protected Health Information (PHI).
Sharing occupational therapy SOAP notes
In addition to therapist access, clients and other clinicians may also need to view occupational therapy SOAP notes. Having a seamless way to send, sign and receive notes in a secure environment helps ensure HIPAA compliance and provides a great client experience.
Sharing
- Secure sharing of occupational therapy notes: TheraPlatform's EMR eases secure sharing of occupational therapy notes with clients through a HIPAA-compliant client portal. Grant clients convenient access to their notes for personal records or insurance audits while ensuring confidentiality and privacy.
- Electronic signatures: Through our Pro and Pro Plus plans, occupational therapists can request electronic signatures directly on occupational therapy notes. Clients can effortlessly download and print the signed documents, eliminating the need for physical signatures and paper-based processes.
- Integrated E-faxes: TheraPlatform's integration with efax services streamlines communication and eliminates the need for separate platforms when sending or receiving SOAP notes. With a simple click of a button, therapists can seamlessly send and receive faxes directly from TheraPlatform, reducing administrative tasks and enhancing efficiency.
Utilizing an EHR for occupational therapy SOAP note creation, storage and sharing is an easy decision and can save therapists time and frustration.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
TheraPlatform is an all-in-one EHR, practice management, and teletherapy software built for therapists to help them save time on admin tasks. It offers a 30-day risk-free trial with no credit card required and supports different industries and sizes of practices, including occupational therapists in group and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice