Therapy Goals Occupational Therapy
Occupational therapy goals

Occupational therapy goals are essential for reimbursement and help OTs articulate their distinct roles and proposed outcomes to caregivers, clients, and colleagues. Effective occupational therapy goals help payors analyze therapy outcomes and reinforce the efficacy of occupational therapy intervention. Occupational therapy goals also align intervention with clinical problems to streamline information for your plan of care summary, treatment planning, and the reporting process. This article will discuss the elements of creating effective goals and support your client’s success in completing their treatment plan.
Setting occupational therapy goals
Goals address the “who, how, what, when, and where” of a treatment plan. Before therapists can create goals, they must collect information through completing an occupational profile, observational assessment, client self-report questionnaires, standardized assessments, and reviewing a past medical history. The occupational profile helps anchor the evaluation to the client’s perspective, priorities, and activities that need improvement. Once the occupational profile is complete, standardized assessments and observational data will measure objective data to add more structure to your evaluation. Once you have all the information and data recorded, it’s time to create a treatment plan with Long-Term (LTG) and Short-Term (STG) goals.
What are SMART goals for occupational therapists?
SMART goals have historically been used as a model for goal setting to ensure occupational therapy goals are complete and measurable. A SMART goal is an acronym for goals that consists of five essential factors: Specific; measurable; attainable; relevant; and time-based.
Specific: This section refers to the tangible outcome. What does the client want to do? For example: Laurie will complete a 5-step task of making tea; Aaron will cut out a circle using both hands; Mary will wash her hands completely. Be sure that you know the client’s current level of performance, and conditions such as using functional form or if they are in a seated position.
Measurable: This piece is essential for both reimbursement and tracking progress. It gives concrete data on the degree of the client’s performance. The measurable piece of a goal can come in different forms: Duration (within five minutes); pain level (client reporting a maximum pain level of 4/10); portfolio collection (for something tangible the client created); client satisfaction (using the Canadian Occupational Performance Measure).
Attainable: Consider how much time you have with the client along with their current level of functioning. Can the client re-learn to tie their shoes in their short acute care stay? Likely not. However, the same client may be able to wash their hands with a visual aid and no more than one verbal cue.
Relevant: An essential component for occupational therapy, it is important to ensure that your client wants to reach their goals. Motivation can have an enormous impact on progress. While the process of coming up with relevant occupational therapy goals begins with incorporating a client’s occupational profile and involving them in the goal creation process.
Time-based: How long will it take to attain these goals? Examples include, “within five days,” “at the time of discharge,” or “by April 1, 2022.” The time given will vary by clinical setting. In an acute care setting, goals may be written for three days. Inpatient rehab goals could be several weeks long. In the educational system, students who have an IEP often have goals written for an entire year.
A client-centered approach, especially during goal setting, involves the clients and caregivers during the therapeutic process, giving them a central and active role in their care. Studies suggest that clients have improved satisfaction with occupational performance compared to alternative interventions. Strategies for assessing client needs and abilities include using the Canadian Occupational Performance Measure and creating an occupational profile template to help gather information.
Types of occupational therapy goals
Long-term goals describe what the client should be able to do by discharge. This timeframe will vary from a few days in acute care to several months in outpatient or even a year in the school setting. There are typically about 2 to 3 short-term goals supporting each long-term goal as mini milestones to help the therapist, client, and payor see the progress achieved while working toward long-term occupational therapy goals.
Short-term goals help track progress as therapy progresses and are reviewed frequently through a client’s plan of care. Both long term and short-term goals are updated by the supervising therapist periodically to reflect any changes in functional stages or to demonstrate progress made.
What are occupational therapy goals examples?
Physical occupational therapy goals example:
LTG: Client will independently complete grooming routine during 5/5 trials, demonstrating functional strength and ROM in right shoulder to wash and style her hair in a standing position, using compensatory strategies as needed in 6 months, by 1/29/24.
STG: Client will report being able to complete grooming routine with minimal assistance during 3/5 trials, with use of compensatory strategies as needed at least 3/5 strength in right shoulder in 3 months, by 10/29/23.
Cognitive occupational therapy goals example:
LTG: Client will independently prepare coffee, during 5/5 trials, demonstrating functional cognition and safety awareness, using compensatory strategies as needed within 6 months, by 01/29/24.
STG: Client will demonstrate ability to complete retrieval of 5/5 items independently in preparation for making coffee, demonstrating improved memory, and attention, using compensatory strategies as needed within 3 months, by 10/29/23.
Self-care occupational therapy goals example:
LTG: Client will independently complete home management task with 95% accuracy, demonstrating improved functional mobility to vacuum, 3 rooms with 0x loss of balance, Assistive devices as necessary within 6 months, by 01/29/24.
STG: Client will demonstrate ability to independently vacuum 1 room of home, with 0x loss of balance and initiation of energy conservation techniques as needed within 3 months, by 10/29/23.
Work-related occupational therapy goals example: It is especially helpful to review job descriptions and requirements when considering writing these goals.
LTG: Client will demonstrate improved divided attention to independently complete at least 6 hours of light duty office work with 0x errors, using compensatory strategies and Assistive devices as needed within 6 months, by 01/29/24.
STG: Client will demonstrate ability to complete at least 3 hours of light duty office work with stand by assistance, 0x errors, and use of compensatory strategies and assistive devices as necessary to maintain safety within 3 months, by 10/29/2023.
Implementing occupational therapy goals
Use these strategies for incorporating occupational therapy goals into treatment plans:
Don’t write occupational therapy goals that you do not have baseline data for. Without this foundation you will not know what criteria to add for your client or if the goal is attainable or even necessary. This would also provide a significant challenge for writing progress notes.
Don’t assume that an ADL or IADL is meaningful to your client. While a grocery shopping goal can encompass many of the skills that your client is working on, they may greatly prefer to order their groceries to be picked up.
Make sure your occupational therapy goals are client centered, with focus on occupations identified as meaningful to your client.
Prioritize and separate important occupational therapy goals into unique objectives. For example, rather than “use a dynamic tripod grasp to draw a 5-part person” , create one objective for grasp and another objective for visual motor skills.
Do create a system for tracking data over time. This may look like a visual representation on graph paper or computer software that automatically generates a visual as you input numerical data.
Tips for motivating clients to work towards their occupational therapy goals
Health literacy refers to the ability to access, evaluate, understand, and communicate health information to promote, maintain and improve health and well-being. Health literacy is directly related to the efficacy of your treatment plan by writing occupational therapy goals your clients not only find meaningful, but clearly written and respectful of diverse cultural values.
Health literacy also plays a role in cultural competency as limited health literacy is recognized by the National Library of Medicine as contributing to racial/ethnic disparities experienced throughout health care and limited access to health care services.
Furthermore, evidence supports that providers who respect health literacy and cultural differences can improve patient adherence and health outcomes.
Recognize challenging health literacy situations and make adaptations as needed to ensure your client understands and believes in the information you are providing them.
Standardize, regulate, and organize your interventions. Organize intervention so that it makes sense on paper to your clients, their caregivers, and other members within the healthcare team. Systematically include health literacy opportunities to engage your clients and continue increasing their health literacy knowledge.
Make information accessible. Reflect on your communication. Do you communicate your ideas clearly? Make sure you talk and educate in clear, direct language versus using a word salad of technical terms that may clutter the point you are trying to make.
Strengthen interactions. Review current literature to keep your clients engaged with the interventions and implement modern strategies with supported evidence to enhance efficacy of your interventions.
Identify health literacy opportunities to recognize when a client may not understand the health information. Identify the barriers and intervene to improve limitations to health literacy.
Review public health literature and work as a network with other professionals to reach the overall goal of improving the patient’s condition management.
Emphasize empowerment, self-confidence, feelings of personal efficacy, being in control, and a range of skills like reading and writing. These characteristics give individuals more control over their health and environment to make healthy choices in their life.
Provide effective patient and family education. This includes asking for feedback to ensure clients and families understand the education, and if they believe the education or recommendations will work for them. Also work with clients and families to include realistic expectations for implementing education as they work toward their occupational therapy goals.
Measuring progress towards occupational therapy goals
Measurable and specific occupational therapy goals help identify progress achieved and help your clients see progress from their hard work in therapy. Incorporate standardized questionnaires periodically to measure your clients perceived difficulty level, pain, or skills level for activities to track changes in their status.
Performance-based assessments allow the therapists to set up standardized environments to measure client skill levels. Together, self-report questionnaires and performance-based measures help provide a well-rounded picture of client participation and engagement. Another important factor to consider is who will track the data? Sometimes therapist collection of data is sufficient but where carryover is essential, the therapist may want to designate a teacher, health professional, or caregiver to track the data.
Adapting occupational therapy goals for different populations
Occupational therapy goals are adapted to meet the needs of each client for different populations. Goals for children may include incorporating family, teachers, and social interactions with the child and highlighting developmental skills to demonstrate improved independence. Empower older adults and people with different abilities by listening to their goals and using strategies such as motivational interviewing to look further into creating meaningful activities to increase their engagement in occupations.
Assistive technology enables people with different abilities to lead independent lives. Assistive technology includes everything from home technology, smartphone apps, prosthetic devices, adaptive equipment, and home modifications that support living independently. Examples include using switches for wheelchair mobility or a smartphone app to support memory that clients can use independently in their daily routines. The use of assistive technology requires collaboration with clients to ensure health literacy is functional and assessed for true efficacy if the device achieves improved participation and meets the client's needs. Incorporate assistive technology tools into occupational therapy goals as clients become independent in managing the assistive technology to achieve independent participation in their daily routine.
Start 30-day Free Trial and explore TheraPlatform. HIPAA Compliant Video and Practice Management Software for Therapists.
Creating meaningful occupational therapy goals is essential for client motivation, tracking progress, and getting reimbursed. By listening to your client and creating effective goals, you can ensure that your client’s goals have all the necessary components for them to be successful. Suggestions for further reading and resources to learn more about occupational therapy goals include visiting the following organizations to look up variations of keywords such as “health literacy” “motivational interviewing” and “occupational therapy goal setting” for more information.
Improve the occupational therapy goals process with EHRs
Therapy goals are critical in occupational therapy treatment plans, providing concrete expectations and guiding clients to excellent outcomes. Efficiently monitoring goals for multiple clients can be challenging without the right tools. Fortunately, Theraplatform offers an all-in-one EHR, practice management, and telehealth tool specifically designed for occupational therapists to streamline the process and save valuable time in managing occupational therapy goals.
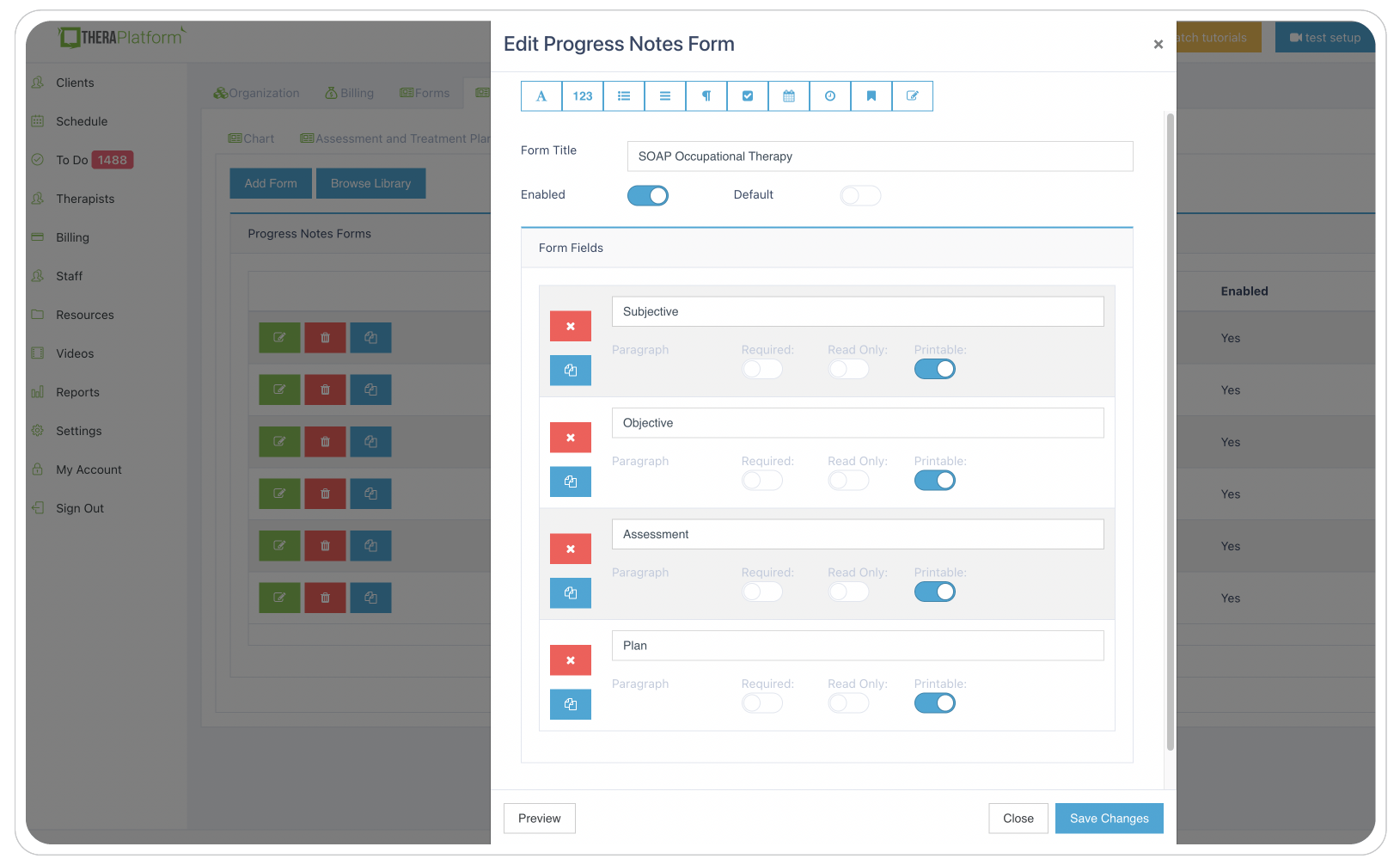
Sample screenshot of progress documentation available to occupational therapists on TheraPlatform.
A comprehensive assessment, treatment plan, and therapy note library: Theraplatform offers a built-in library of assessments, treatment plans, and therapy notes to streamline the process of creating occupational therapy goals and assessments. These resources can be easily modified to align with the specific requirements of each practice. Therapists also have the flexibility to create customized templates using Theraplatform's form builder, ensuring personalized and tailored goal-setting.
Top occupational therapy goals features of Theraplatform:
Personal bank of goals, objectives, and interventions: Theraplatform automatically saves newly entered goals, objectives, and interventions to eliminate repetitive data entry. Using a personal bank of previously entered information allows therapists to easily reference and use data for each client, ensuring consistency and efficiency in goal-setting.
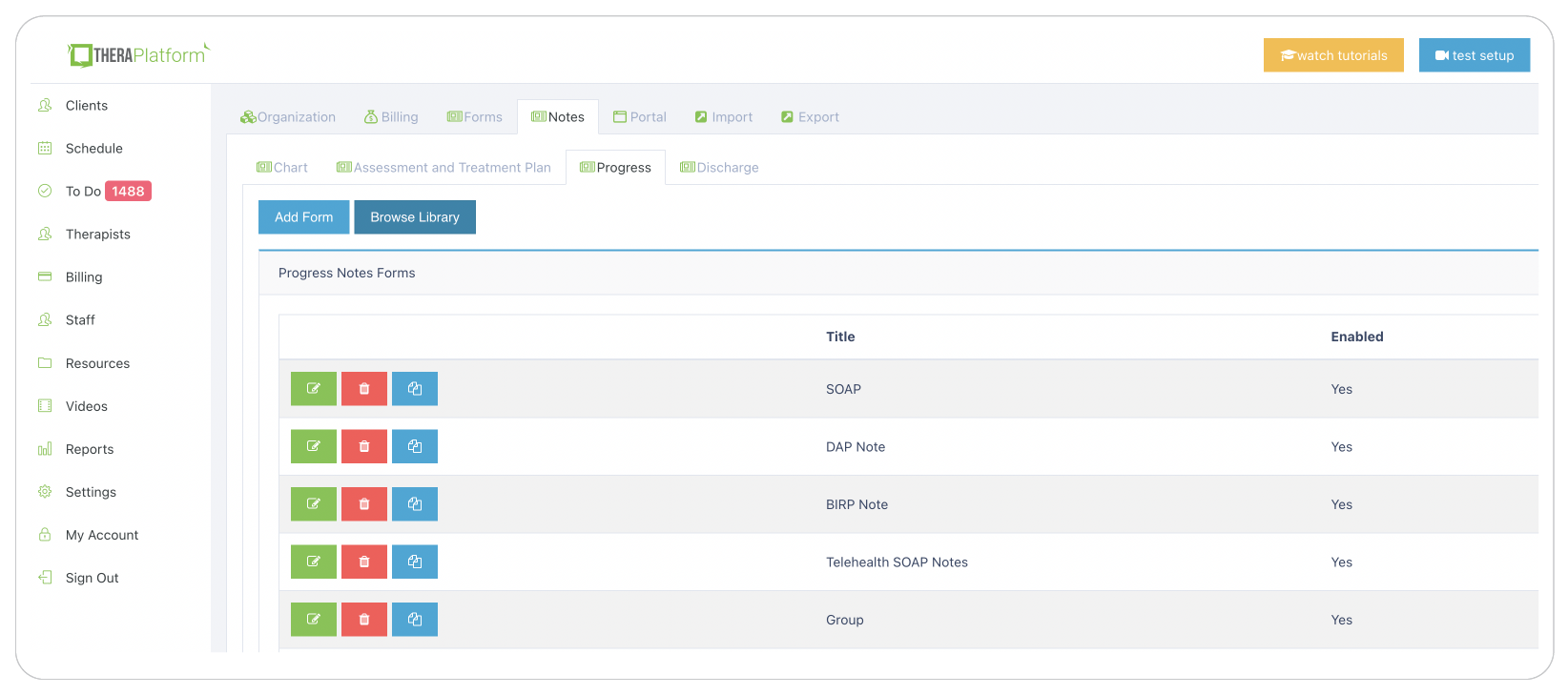
Sample screenshot of library with various documents available to occupational therapists on TheraPlatform.
Goal monitoring: Enter occupational therapy goals and conveniently monitor progress after each session is easy with TheraPlatform. Link goals directly to therapy notes and track clients' progress over time. The platform also offers scored visual representations of therapy goals in graphs, providing valuable insights into clients' development and informed decision-making for their treatment.
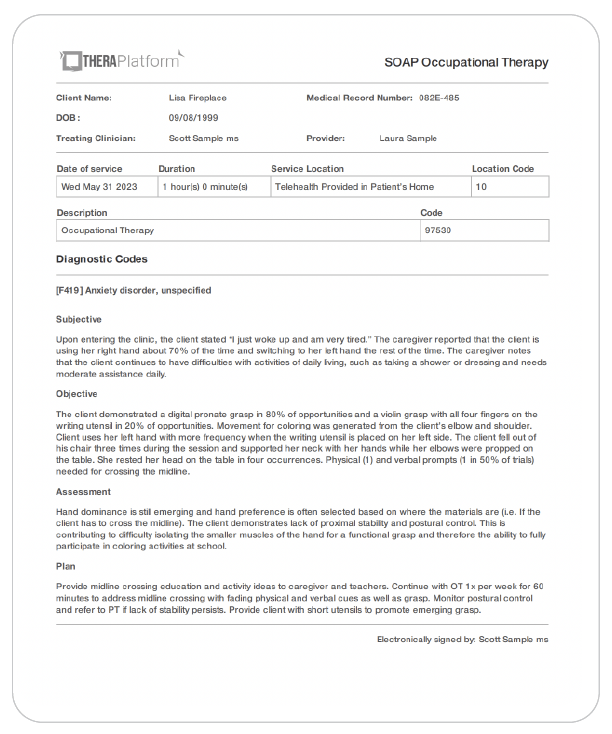
Sample screenshot of occupational therapy SOAP note created with TheraPlatform.
Using Theraplatform's comprehensive EHR solution, occupational therapists streamline the process of setting and monitoring therapy goals. With features like a personal bank of goals, a library of assessments and therapy notes, and goal monitoring capabilities, Theraplatform empowers therapists to provide more efficient and effective care, ultimately improving client outcomes in occupational therapy.
TheraPlatform is an all-in-one EHR, practice management and teletherapy tool that can help you navigate the complexities of billing and help you to maintain the information you need. They offer a free, 30-day trial with no credit card required. Cancel anytime.
Resources
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice