How to test and implement AI for therapy notes

AI for therapy notes is becoming a more common practice for providers as they face not only the demanding complexities of clinical care, but also a substantial administrative burden.
Summary
- AI tools help automate progress notes, transcriptions, and session summaries—freeing up therapists’ time and reducing stress from administrative overload.
- AI enhances documentation quality by standardizing clinical language, flagging missing fields, and helping ensure compliance with billing and legal standards.
- AI-generated notes are drafts requiring therapist review. Human oversight is essential to interpret emotional nuance, cultural context, and therapeutic intent.
- Therapists must choose HIPAA-compliant tools such as TheraPlatform, integrate them into workflows responsibly, and clearly communicate with clients about how their data is used.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

From progress notes and treatment plans to insurance documentation and audit compliance, recording and managing client information consumes a considerable portion of clinicians' time.
Although precise data within psychotherapy remains scarce, broader healthcare trends suggest this burden contributes significantly to clinician fatigue and diminished therapeutic focus.
AI for therapy notes and AI tools present an emerging solution, aiming to streamline workflows while maintaining clinical integrity. To harness their potential effectively, therapists must balance efficiency gains with ethical considerations and clinical oversight.
AI‑assisted progress notes in the mental health practice
AI for mental health therapy notes serve as documentation aides, not standalone clinicians, with key functionalities that include:
- Voice-to-text transcription: Speech recognition and natural language processing (NLP) convert therapy session recordings or live dictation into draft documentation, tailored toward clinical terminology.
- Session summarization: Advanced NLP models distill session content into structured summaries that capture key themes, mood shifts, and client statements, often outperforming generic models when trained specifically on therapy dialogue.
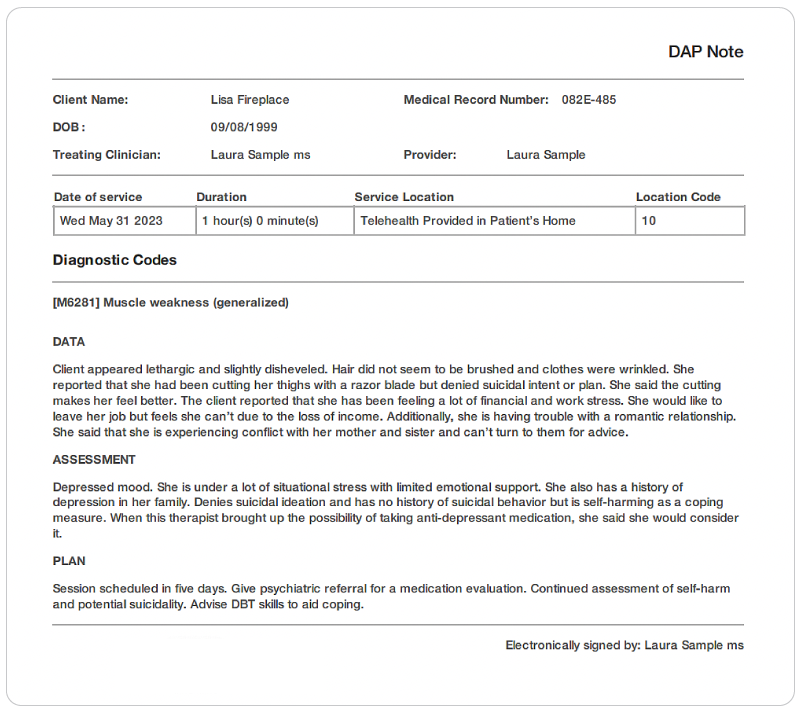
- Template-based generation: These tools can automatically populate formats such as SOAP, DAP, or BIRP based on session content, reducing manual input and increasing consistency.
- Clinical language guidance: Some systems suggest phrasing that aligns with clinical standards, helping ensure accuracy and uniformity across documentation.
Yet, AI outputs remain drafts: Therapists must review them to ensure accuracy, interpret emotional nuance, and detect subtleties like sarcasm or dissociation that AI may miss.
Practice Management + EHR + Telehealth
Manage more in less time in your practice with TheraPlatform

Evidence‑based benefits of AI for therapy notes
Using AI for therapy notes has rapidly gained traction in mental health settings, and emerging research suggests they offer several meaningful benefits for both clinicians and clients.
One of the most widely recognized advantages is improved efficiency. In various clinical environments, studies have shown that utilizing AI for therapy notes significantly reduces the time therapists spend writing notes.
AI for therapy notes may save time and reduce burnout
By automating repetitive tasks and generating structured drafts, these tools lighten the mental load of documentation and free up more time for direct client care or administrative responsibilities. This reduction in clerical work not only streamlines the workflow but also helps practitioners stay on top of compliance demands without sacrificing personal time or energy.
The reduction in documentation time has also been linked to lower levels of clinician burnout. Mental health professionals often report stress related to late-night note writing or the pressure to complete documentation between back-to-back sessions.
Using AI for therapy notes can assist with or automate portions of this process and decrease this strain, supporting better work–life balance, helping therapists preserve their emotional bandwidth for client care. While AI is not a replacement for clinical judgment, it acts as a reliable support system that reduces the burden of administrative overload.
AI for therapy notes may improve consistency and accuracy
Beyond time savings, using AI for therapy notes contributes to greater consistency and improved quality assurance. They can help standardize language across progress notes, ensure required fields are completed, and even flag inconsistencies or gaps that may affect compliance or reimbursement. This built-in quality check not only improves the reliability of clinical records but also provides a safety net that supports billing accuracy and legal defensibility.
Increased therapeutic presence
Another notable benefit reported by clinicians is an increased therapeutic presence. With AI handling much of the documentation workload, therapists can remain more engaged during sessions, without the distraction of having to track every detail for later documentation mentally. This fosters a more attuned therapeutic relationship, allowing for deeper connection, better listening, and greater responsiveness to the client's needs in the moment.
Together, these benefits highlight how thoughtfully integrated AI tools can enhance, not replace, the human elements of care, ultimately supporting therapists in delivering more focused and effective treatment.
AI notes for therapists
Watch this video to discover 3 smart ways AI can speed up your note-taking
→ Start My Free Trial - Save Hours on Notes Starting Today
Key considerations when selecting an AI tool
Clinical customization: Select an AI tool specifically designed for mental health professionals. Generic platforms may miss the mark when it comes to understanding therapeutic approaches, trauma-informed language, or the cultural nuances that shape client care. Look for tools that reflect the diversity of clinical practice, support different modalities, and avoid overly medicalized or pathologizing phrasing. A well-calibrated tool can enhance your documentation without compromising your therapeutic voice.
Security and compliance: Privacy and legal compliance are crucial when dealing with sensitive client information. Your chosen tool should meet HIPAA standards or the equivalent in your region. Features like end-to-end data encryption, clear data retention policies, and the option to sign a Business Associate Agreement (BAA) should be non-negotiable. Transparency in how data is stored, accessed, or used for AI training is also essential to maintain ethical standards and protect your clients.
Workflow integration: An AI tool should streamline your work, not create additional steps. Prioritize platforms that sync smoothly with your existing systems, including your electronic health record, calendar, billing software, and client portals. These integrations help reduce redundancy and improve overall efficiency, allowing you to focus more on client care and less on administrative burden.
Therapist oversight and control: Therapist autonomy must remain fundamental. The best AI tools provide suggestions, not mandates. Ensure you can freely edit, accept, or discard AI-generated content and that you have the option to turn off automated features. Choose platforms that explain how outputs are generated so you can stay informed and maintain full clinical authority.
Free Resources for Therapists
Click below and help yourself to peer-created resources:

Ethical and legal imperatives in using AI for therapy notes
Transparent informed consent: Informed consent is a critical ethical requirement when incorporating AI into documentation or client interactions. Clients have a right to know how their information will be processed, including whether artificial intelligence tools are being used to generate or summarize notes. This conversation should happen early in the therapeutic relationship and be revisited periodically as technology or policies change. Clients must be allowed to decline AI involvement in their records without it affecting their access to care. Clear, respectful communication fosters trust and respects client autonomy.
Guarding Against Over-Reliance on AI: While AI tools can significantly reduce administrative workload, therapists must stay deeply engaged in their clinical reasoning. There's a risk of letting AI-generated text override or dilute the nuanced, human aspects of therapy, especially when note content becomes templated or overly uniform. Ethical practice demands that therapists continue using their clinical judgment and tailor documentation to reflect the unique voice, culture, and experience of each client. Regular review and personalization help preserve the therapeutic relationship and prevent depersonalization.
Cultural and linguistic sensitivity: AI tools are not immune to bias. Many models have been trained predominantly on Western, English-language data sets, making them prone to misinterpreting cultural references, dialects, or expressions from non-dominant populations. This limitation can result in microaggressions, inaccuracies, or omissions in documentation. Therapists should perform ongoing qualitative review of AI output to ensure it remains respectful, relevant, and appropriate to the client's background and identity. Integrating cultural humility into AI use is a necessary safeguard against systemic bias.
AI for therapy notes implementation
Pilot testing before a full rollout: Initiate a short-term trial period—typically around three months—before adopting an AI documentation tool across your practice.
Select one or two promising platforms and assign a small group of clinicians to use them during this phase.
Monitor key performance indicators such as documentation time, quality of notes, and perceived workload. This comparative data can provide a concrete basis for long-term decision-making and help you uncover unforeseen implementation issues in a low-risk environment.
Training and documentation protocol design: Provide structured training for all clinicians to ensure clarity around the intended use of AI. Emphasize that AI-generated notes should be viewed as a starting point rather than a final product. Develop clear internal guidelines that outline review protocols, error correction procedures, and expectations for clinician oversight. Encourage staff to report inaccuracies or instances of model "hallucination," which are known limitations of generative AI (Van Dis et al., 2023).
Transparent client communication: Maintain openness with clients by informing them of the use of AI-assisted tools, especially if session content may be recorded or transcribed. This transparency supports client autonomy and promotes trust. Provide precise opt-out mechanisms for clients who may feel uncomfortable with AI involvement, and explicitly explain what information is stored, for how long, and who has access.
Therapist tips for using AI for therapy notes effectively
AI documentation tools offer significant potential to streamline workflows, but their effectiveness hinges on how clinicians use them. Here's how to integrate AI into your practice thoughtfully.
Start with session summaries or voice memos
Begin by using AI to transcribe brief voice memos or draft session summaries. This reduces initial resistance to the technology and lets you evaluate accuracy before scaling up. For example, tools like Eleos Health specialize in behavioral health dialogue, capturing nuances better than generic transcription apps.
Use AI to draft and review for nuance and tone
Treat AI-generated notes as a "first draft." Always review for:
- Emotional tone (e.g., does it misinterpret sarcasm or dissociation?).
- Cultural/language biases (e.g., does it pathologize non-Western expressions?).
- Clinical relevance (e.g., does it prioritize billing codes over therapeutic insights?).
Save templates and prompt styles for frequent cases
Create custom templates for common scenarios (e.g., CBT for anxiety, trauma intake) to maintain consistency. For instance, prompts like "Summarize key themes from this session, focusing on safety planning and coping strategies" yield more targeted results than vague requests.
Use AI insights to enhance treatment planning
Some tools analyze trends across sessions (e.g., mood shifts, frequently used coping skills). Use these insights—with clinical judgment—to adjust interventions. For example, if AI flags repeated mentions of sleep disturbances, you might explore sleep hygiene more deeply.
The future of AI for therapy notes
AI's potential in mental health goes beyond note-taking. Emerging applications include:
Predictive analytics for early intervention: AI is beginning to play a role in identifying subtle shifts in client language that may suggest emerging risk factors, such as increased suicidal ideation or emotional deterioration. While these predictive insights can support early intervention, they must be paired with human discernment and ethical oversight to avoid inappropriate conclusions.
Enhanced supervisory support: For newer therapists or those in training, AI systems can act as reflective tools, flagging inconsistencies, documentation gaps, or potential areas of bias. Used correctly, this can complement clinical supervision and enhance learning without replacing it.
Dynamic, adaptive templates: Future AI note systems may evolve to adapt their prompts and structure based on ongoing clinical outcomes. For example, a client showing progress in emotional regulation may prompt the system to shift focus toward relational themes or maintenance strategies. These adaptive tools could support more nuanced, individualized note-taking without increasing documentation time.
The human element remains central: Despite the promise of these innovations, it is paramount to remember that AI is a supportive tool, not a substitute for therapeutic presence, empathy, or relational understanding. The clinician's insight, judgment, and connection with clients will always remain the heart of effective therapy. Remember, it is the therapeutic relationship that is at the core of all the best therapy processes.
Improving mental health assessment notes with EHR software
EHR software and practice management tools, such as TheraPlatform, offer numerous advantages in creating accurate, efficient, and organized notes.
Top 7 benefits of using EHR for notes management
Manually writing and storing notes can be cumbersome for many therapists. That process can be further exacerbated by simple document requests that include locating, faxing or scanning documents.
Features like customizable templates, secure storage, easy sharing, duplication, electronic signatures, and eFax integration, streamline the note process, optimizing therapy documentation and workflows.
- Consistent notes with template library: EHRs equipped with a library of note templates enable therapists to create standardized and concise notes quickly. This feature ensures consistency across notes, making it easier to review client progress. Additionally, EHRs provide centralized storage and management of notes, enhancing accessibility and organization.
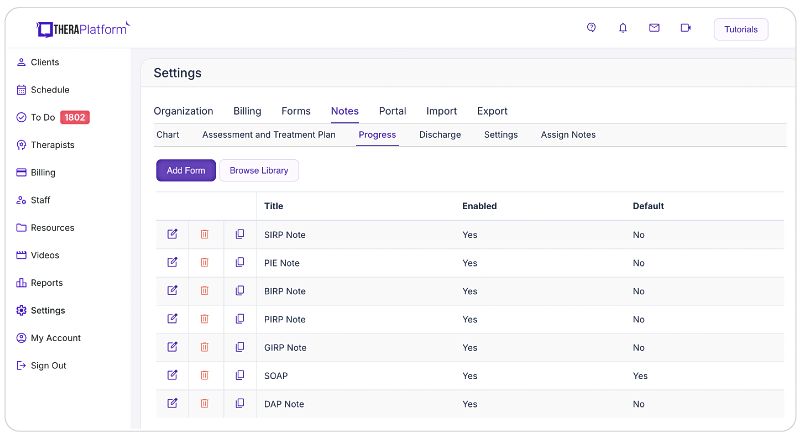
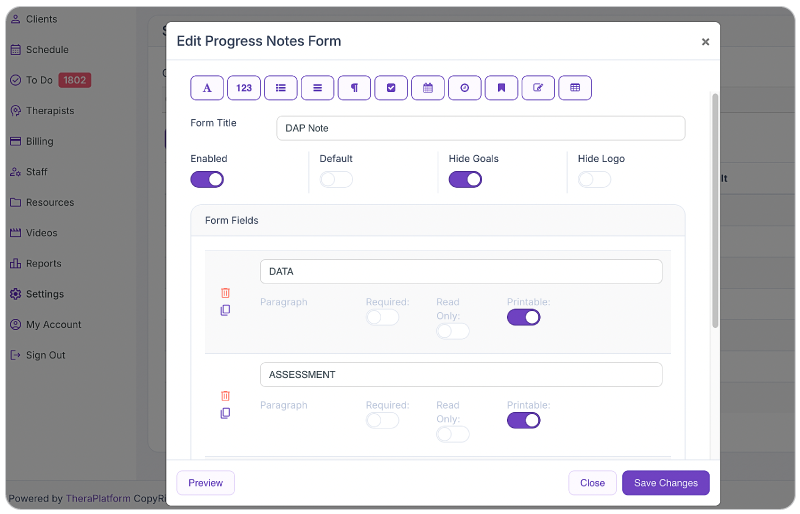
- Customizable notes: Not all EHRs offer customizable note templates tailored to therapists' unique needs. However, with a robust and user-friendly note template builder, therapists can customize note templates to align with their preferred note-taking style. This flexibility allows for efficient data entry, whether therapists prefer separating sections or using a single note field or checkboxes for mental status or techniques.
- HIPAA-compliant note storage: EHRs prioritize data security by implementing bank-level encryption to safeguard notes and other client information. TheraPlatform, for instance, ensures HIPAA compliance by offering signed, legally-binding Business Associate Agreements to protect Protected Health Information (PHI) between compliant entities.
- Seamless note sharing with clients: Clients may request access to their notes to better understand their treatment or keep them for record-keeping purposes. Using an EHR, therapists can securely share notes with clients, saving time compared to paper-based practices. TheraPlatform, a HIPAA-compliant EHR for therapists, facilitates secure note sharing with clients.
- Duplicate notes: In cases where the data remains the same across multiple sessions, duplicating notes can save time. This feature is particularly useful when clients exhibit repetitive behaviors or show minimal progress, allowing therapists to refer back to previous notes for accurate documentation.
- Client signatures made easy: EHRs streamline the process of requesting client signatures. TheraPlatform's Pro and Pro Plus plans enable therapists to request electronic signatures directly on notes. Clients can conveniently download and print the documents requiring their signatures.
- Easier faxing: TheraPlatform offers eFax integration as an add-on feature, eliminating the need for toggling between multiple services. This integrated solution allows therapists to send and receive documents, including notes, via fax directly from TheraPlatform. Additionally, received faxes can be easily filed under the respective client's charts.
By leveraging the capabilities of EHR software like TheraPlatform, therapists can enhance the accuracy, efficiency, and accessibility of their notes, allowing them more time to enhance client care.
Additional tools and outcome measures to help with data collection and progress monitoring
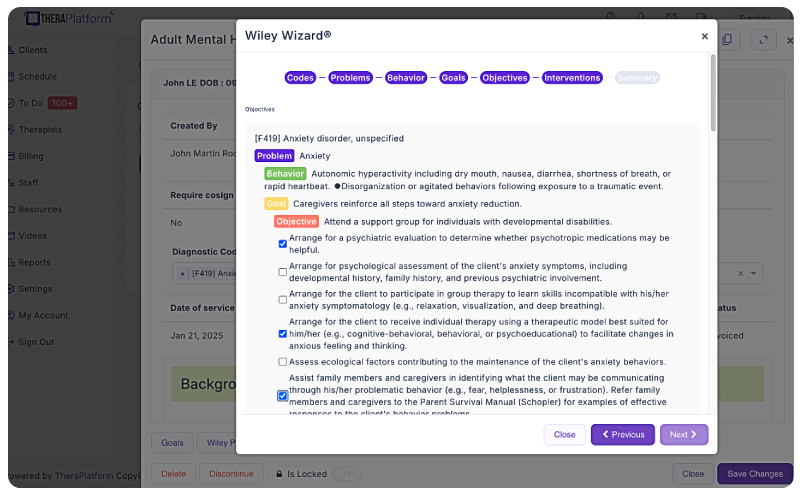
Therapists can also take advantage of EHRs (such as TheraPlatform) that offer integrations with Wiley treatment planners to ensure consistent data collection on progress from session to session. The best part about partnering with a modern EHR is the time you save on formulating the actual notes and scoring.
What is Wiley Treatment Planner?
Wiley Treatment Planner is a widely used clinical resource designed to help mental health professionals and other therapists efficiently create treatment plans for their clients. In addition to treatment plans, the company also provides prewritten therapy notes for some diagnostic codes. It is part of the "PracticePlanners" series published by Wiley.
Features of Wiley Treatment Planner includes:
- Prewritten, evidence-based treatment goals, objectives, and interventions
- Treatment planners tailored to specific populations and problems, including adults, children, adolescents, couples, families, addictions, and more
- Alignment with the diagnostic criteria from the DSM-5 and ICD-10
- Prewritten therapy notes
Is there an online version of Wiley Treatment Planner and how can I get the Wiley Treatment Planner?
Wiley Treatment Planner company partnered with a select number of EHRs for mental health providers to make treatment planners available online. TheraPlatform’s EHR offers the Wiley Treatment Planner as an add-on for both assessment and treatment plans and therapy notes, such as notes. You can edit prewritten notes and add your own with any therapy template on TheraPlatform.
Save time with automatically scored outcome measures
Mental health therapists can use outcome measures to document progress, track a variety of key clinical indicators, helping providers make data-driven decisions, improve communication with clients, and improve client outcomes. Additionally, outcome measures help therapists adhere to compliance requirements and provide documentation needed to support reimbursement.
Watch this video to learn about how to autoscore outcome measures
→ Sign up for a Free Frial
While outcome measures clearly provide benefits to both clients and therapists, they can be time-consuming, especially if clinicians score responses manually.
However, many aspects of outcome measures can be automated through an EHR like TheraPlatform:
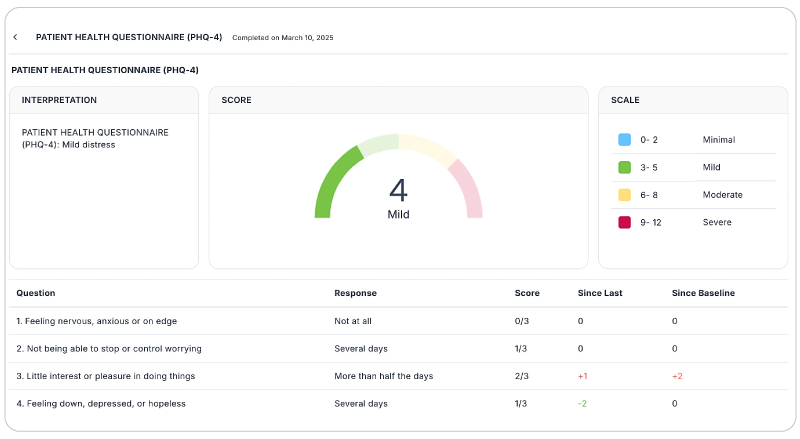
- Sending measurements: Common assessments such as the PHQ-9 or GAD-7 can be automatically sent to clients and stored in their records or they can be scheduled on regular intervals.
- Auto scoring: TheraPlatform automatically scores and sums totals for common outcome measures.
- Report building and analysis: Results can be analyzed over time, with visual charts showing progress on rates of severity and session-to-session progress.
By regularly using these measures, therapists can gain valuable insights, tailor interventions, and improve client outcomes while demonstrating the effectiveness of their care without manual entry.
AI for therapy notes is transforming mental health practice, not by replacing therapists, but by lifting the burden of repetitive tasks. Studies show it can save time, freeing clinicians to focus on what matters: the therapeutic relationship.
Yet, balance is key. AI excels at efficiency; you excel at nuance, cultural humility, and clinical wisdom. The best outcomes arise when technology supports—not supplants—human judgment.
Next steps:
- Test 1–2 tools (e.g., TheraPlatform's free trial) with a pilot group.
- Refine workflows based on what preserves your clinical voice and client trust.
The future of therapy isn't AI or humans – it's AI and humans, working together to deliver care that's both efficient and deeply personal.
Streamline your practice with One EHR
- Scheduling
- Flexible notes
- Template library
- Billing & payments
- Insurance claims
- Client portal
- Telehealth
- E-fax

Resources
Theraplatform is an all-in-one EHR, practice management and teletherapy solution with AI-powered note taking that allows you to focus more on patient care. With a 30-day free trial, you have the opportunity to experience Theraplatform for yourself with no credit card required. Cancel anytime. They also support different industries including mental and behavioral health therapists in group practices and solo practices.
More resources
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
- Mental health credentialing
- Insurance billing 101
- Practice management tools
- Behavioral Health tools
Free video classes
- Free on-demand insurance billing for therapist course
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice
FAQs on AI for therapy notes
Can AI replace my clinical judgment?
No. AI lacks human empathy, contextual understanding, and ethical reasoning. It's a tool to reduce administrative load, not a clinician. As noted in a JAMA Network Open study, AI's role is strictly assistive.
Is it legal to use AI in therapy notes?
Yes, if the tool is HIPAA-compliant (or meets your region's equivalent) and you sign a Business Associate Agreement (BAA). Always verify the vendor's security protocols—end-to-end encryption and audit logs are non-negotiable.
What if a client asks not to be recorded or transcribed?
Respect their autonomy. Offer alternatives:
- Manual note-taking.
- Turning off AI features for their case.
- Document their preference in their records to ensure compliance.
How do I protect client confidentiality with AI tools?
- Avoid free/unvetted tools (e.g., consumer-grade ChatGPT).
- Opt for closed systems where data isn't used to train public models.
- Anonymize inputs (e.g., replace names with initials in prompts).
References
(2025). Apa.org. https://www.apa.org/topics/artificial-intelligence-machine-learning/ethical-guidance-ai-professional-practice
Badawy, W., Zinhom, H., & Shaban, M. (2025). Navigating ethical considerations in the use of artificial intelligence for patient care: A systematic review. International nursing review, 72(3), e13059. https://pubmed.ncbi.nlm.nih.gov/39545614/
Forbes. (2024, August 29). The overlooked documentation burden threatening mental health services. Forbes. Retrieved from https://www.forbes.com/sites/forbeseq/2024/08/29/the-overlooked-documentation-burden-threatening-mental-health-services/ Forbes
JAMA Network Open. (2025). Clinician experiences with ambient scribe technology to assist... JAMA Netw Open. Retrieved from https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2830383 JAMA Network
Mass General Brigham / Peterson Health Technology Institute. (2025, March 27). Early evidence shows AI scribes reduce burnout, but without financial improvement. Axios. Retrieved from https://www.axios.com/2025/03/27/ai-scribes-reduce-burnout-financial-improvement Axios
Srivastava, A., Suresh, T., Peregrine, S., et al. (2022). Counseling summarization using mental health knowledge-guided utterance filtering. arXiv preprint. Retrieved from https://arxiv.org/abs/2206.03886 arXiv
Adhikary, P. K., Srivastava, A., Kumar, S., et al. (2024). Exploring the efficacy of large language models in summarizing mental health counseling sessions: A benchmark study. arXiv preprint. Retrieved from https://arxiv.org/abs/2402.19052 arXiv
Improving clinical documentation with artificial intelligence. (2025). PMC. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11605373/ PMC
Tun, H. M., Rahman, H. A., Naing, L., & Malik, O. A. (2024). Trust in AI-Based Clinical Decision Support Systems Among Healthcare Workers: A Systematic Review (Preprint). Journal of Medical Internet Research. https://doi.org/10.2196/69678



