Therapy notes for telehealth

Therapy notes, also known as progress notes, document what occurs during a therapy session and is added to the client’s record. Therapy notes give therapists the opportunity to record important and necessary information regarding the client, your treatment interventions, the client’s response, and any progress in treatment.
In this article we will cover specific information related to therapy notes in a telehealth session including:
- The different types of therapy notes
- How the notes may be utilized in your practice
- What components to include in your therapy notes
- Legal and ethical considerations
Guidelines to consider when writing your therapy notes for telehealth
When writing your therapy notes, you should demonstrate your observations of the client during the session, how your treatment interventions addressed the presenting issues, and how the client responded.
Your notes should be:
- Clear and concise (so another reader can understand them)
- Accurate
- Objective (only include the facts and stay away from words like “appears” and “seems”)
- Organized (easy to read and follow)
- Well-written (no spelling or grammatical errors, no typos)
- Include the most relevant information (for the reader and to remind you before the next session)
- Only use approved abbreviations
What are the types of therapy notes in telehealth?
When you work for an agency, an employer, or another therapist, you may not have much choice in the format you use for your therapy notes. When you have your own practice, you can decide which type of therapy note you prefer to write.
Most therapists choose from three main types of therapy note formats:
- SOAP Notes or Subjective-Objective-Assessment-Plan
- BIRP Notes or Behavior-Intervention-Response-Plan
- DAP Notes or Data-Assessment-Plan
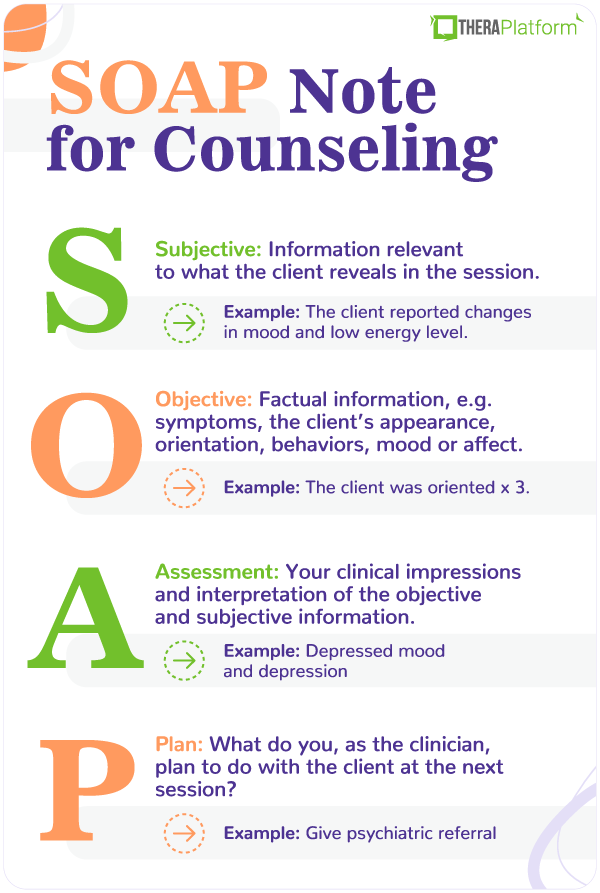
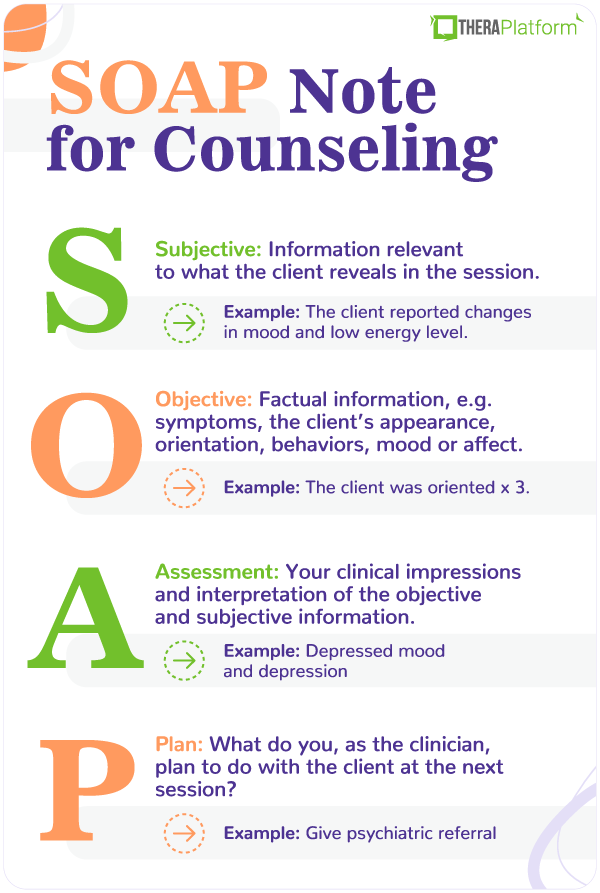
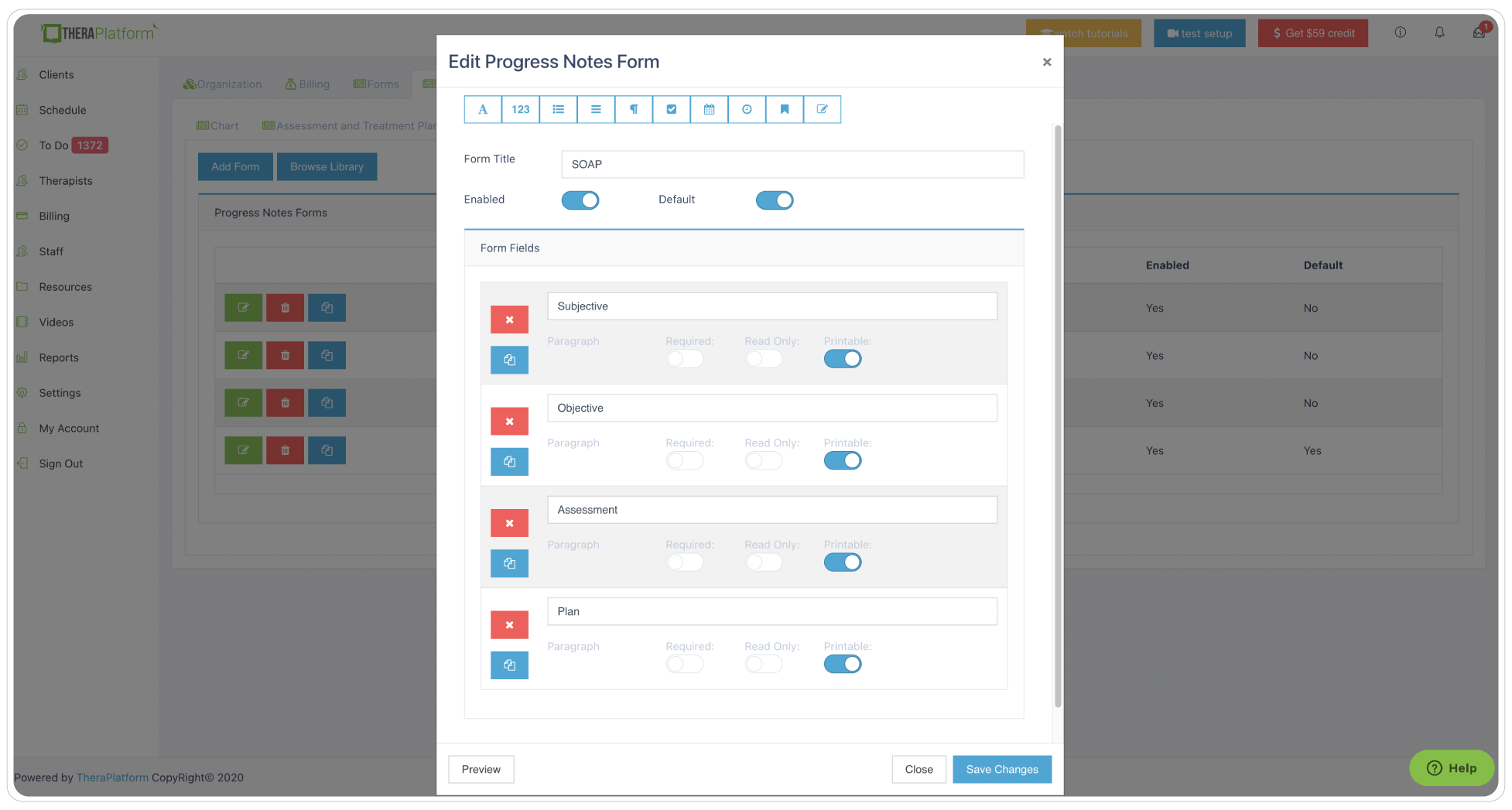
SOAP notes for telehealth
SOAP notes consist of four components:
- Subjective: This section should include the client’s description of their symptoms, issues, and reasons for seeking therapy. You can write direct quotes from the client or restate their words related to their concerns introduced in the session.
- Objective: This component includes the objective data regarding your client. You can include the mental status examination here and any other observations.
- Assessment: In this part of the note, you would synthesize the subjective and objective data from the session. You can include information regarding the diagnosis, a description and describe the goals addressed, and interventions you utilized in the session. If you utilized any assessment tools or reviewed homework from the previous session, you can include a discussion here.
- Plan: In this section of your note, you would include your plan for the next session, any homework assigned to the client, or other follow-up information. You can include the date and time of the next session.
SOAP notes example
BIRP notes for telehealth
BIRP notes have a heavier focus on the client’s behavior.
A BIRP note includes:
- Behavior: In this section, therapists write about the main issue or problem addressed in the session. You should include information regarding the client’s appearance, using both subjective and objective observations in this section.
- Intervention: This part of the note includes a detailed description of what treatment interventions you applied during the session to help the client work towards treatment goals.
- Response: In this component of therapy notes, you can discuss how your client responded to the session and treatment interventions. You can write specific quotes or observations that you made regarding how the client changed as a result of the session.
- Plan: You would write in this section what you plan for the next session, any homework assigned, or follow-up needed. You can record here the date and time for the next session.
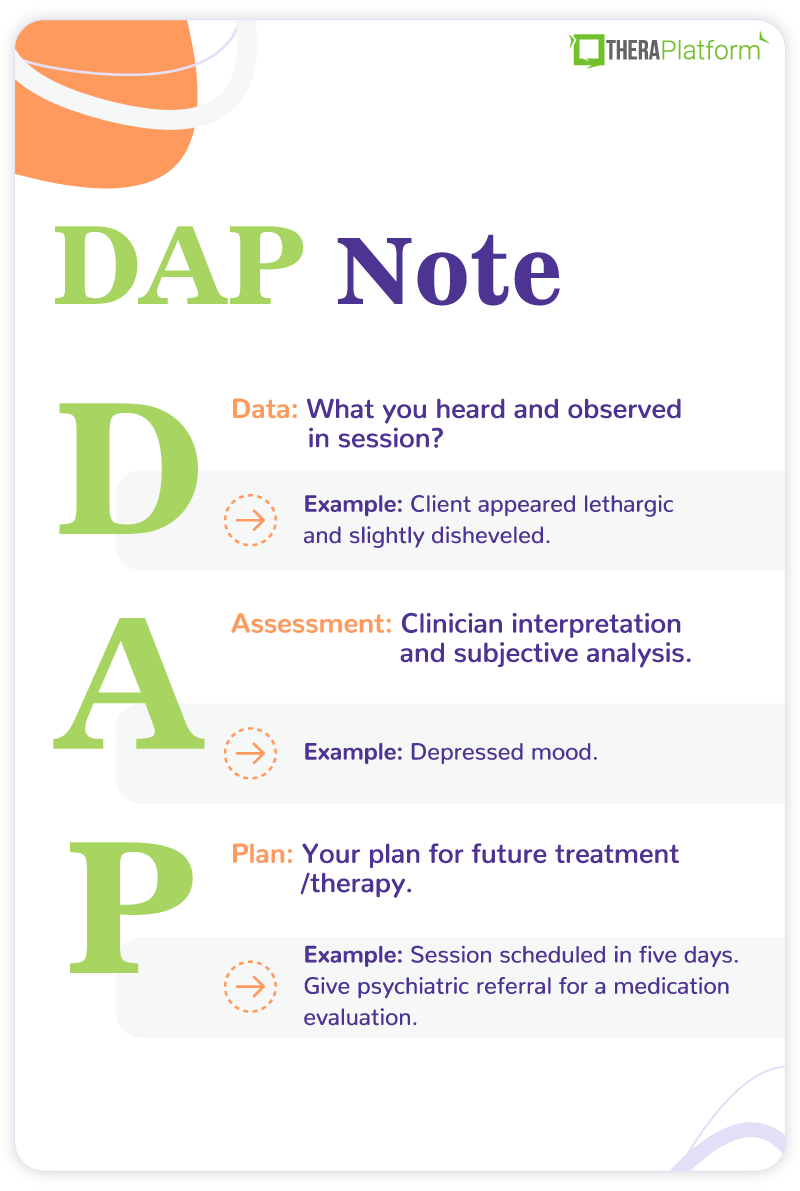
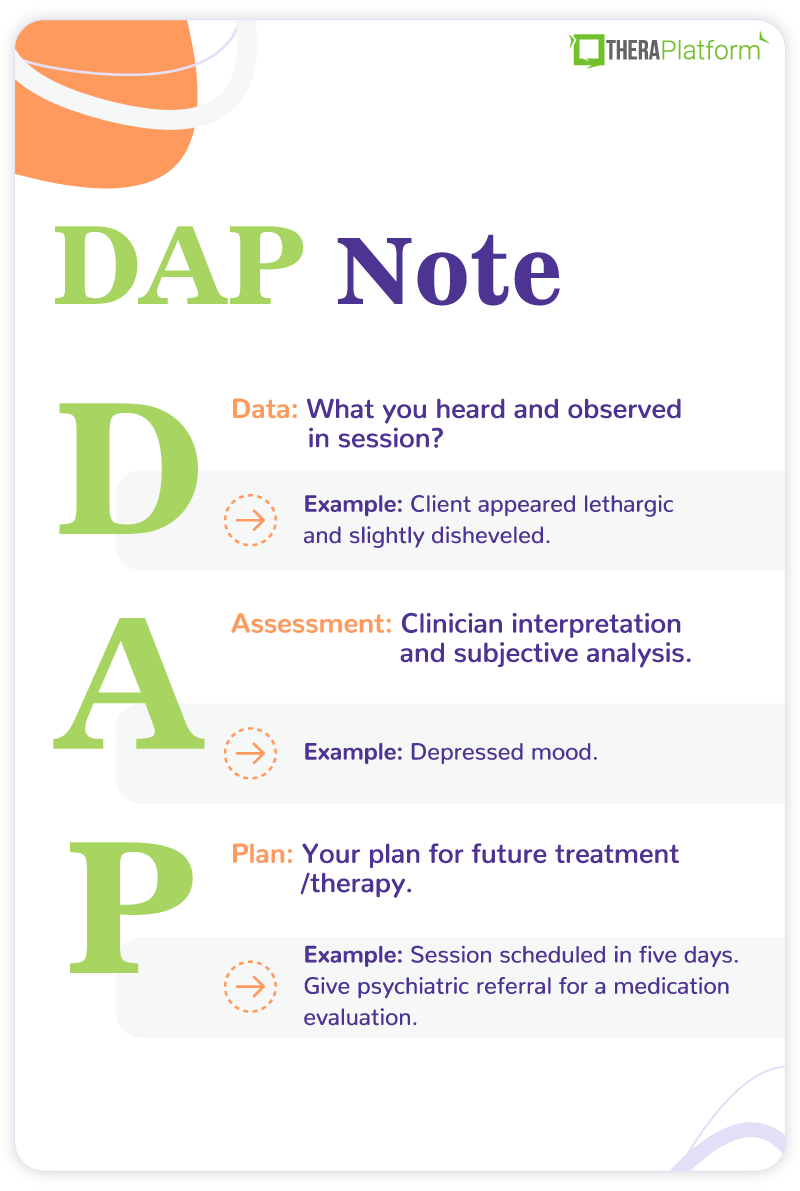
DAP notes for telehealth
DAP notes utilize three sections:
- Data: The data section documents the problems or issues addressed in the session as well as the subjective and objective observations of the client during the session. You would include any descriptions of behaviors or direct quotes from the client. You could also include a mental status exam here.
- Assessment: In this section, document the clinical significance of the observations described in the data section. Describe how the client responded to treatment interventions utilized in the session.
- Plan: Use this component to write about your plan for the next session, any homework, or follow-up plans. You can include the date and time for the next session.
DAP notes example
Components of a therapy notes for telehealth
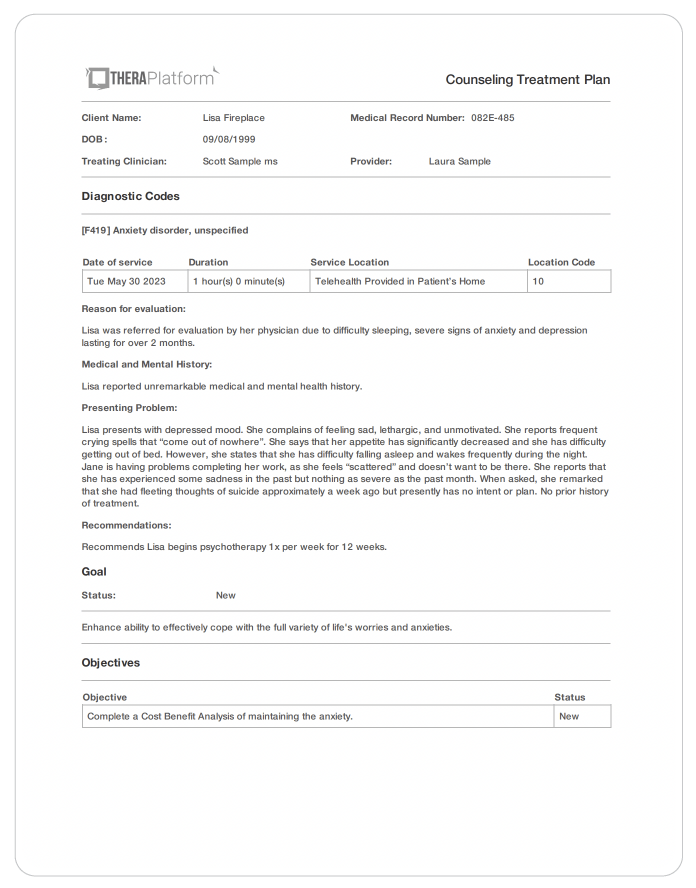
Components of therapy notes will likely vary to some degree based on differing requirements in each state, professional licensure guidelines, modality of therapy, and any third-party payor requirements.
Most electronic health records (EHR) utilize templates that likely include the important components. This function of an EHR helps to ensure compliance with most standard requirements for therapy notes.
As a guideline, most therapy notes should include:
- Client name and another identifier such as case number or date of birth
- Session information (date, exact start and stop time of the session)
- Name and signature of the therapist providing the session
- Who participated in the session (client, family, spouse, etc.)
- Telehealth sessions should include the location of the client (home, etc.) and the type of telehealth (video, telephone)
- An in-person session should include the location as well (office, client’s home)
- Client’s appearance, behavior, and presenting symptoms (you can use a mental status exam type format)
- Diagnosis
- Presenting problems, challenges, or issues addressed in the session
- Treatment goals and objectives addressed in the session
- Safety assessment and safety plan if necessary
- Any reported changes in medications
- What the therapist did in the session, treatment interventions implemented, techniques used, handouts given to the client
- How the client responded to what transpired in the session
- Client’s progress on treatment goals
- Plans for the next session
- Homework
- Any referrals given to the client
- Any follow-up the therapist plans to do (ex.: call the psychiatrist)
- Date and time of the next session
Therapy notes for telehealth sessions
For a telehealth session, a therapist needs to collect additional information and document in the therapy notes. With a telehealth session, you do not have the same control over the environment as you do when meeting with a client in your office. Therapy notes should demonstrate that you have taken precautions for the sessions.
A therapy notes telehealth session progress note should also contain the following specific information:
- Verification of client’s identity: Because the client is not coming to you in your office, you should take measures during the intake session to verify that the client is actually who they say they are. You may ask the client to show an identification card on the video. Then, document your measures on the note.
- The client’s location: Document in the therapy notes the location of the client during the session in case you need to call for emergency assistance. If the client is at the home address or another address listed in your client record, refer to that location. If the client logs onto the session from a different location, then you need to document the new location and address.
- Verification that the client’s location for the session is safe and appropriate: When you have a session in your office, you have control over the environment. However, during a telehealth session, you lack control over what may be going on during the session in the client’s location. You can document on the therapy note that you have verified that the location is safe and appropriate for therapy.
Some measures to assess and document are:
- No harmful or dangerous people such as an abusive partner are in the room
- No distractions
- No one is listening to the session
Plans to address safety, technology, or emergency issues: Part of your intake session can include how you will address any issues that arise during the session. You should document this information as part of your initial session. On your therapy notes, you can include that no changes have been made to the plan or write about any changes that you have made.
Statement of appropriateness for telehealth sessions: Not all clients are appropriate for a telehealth session. As part of your intake assessment process, you want to address this issue and document it accordingly. You can refer to this appropriateness for telehealth in each successive therapy progress note.
Start Your Free Trial Now
Uses of therapy notes in a telehealth practice
Therapy notes have multiple purposes. They demonstrate the medical necessity of your treatment for insurance companies, communicate relevant information to other health care providers to improve continuity of care, and help the therapist to track progress and plans for treatment.
How do therapy notes support medical necessity when billing insurance?
When billing insurance, your therapy note serves as a stand-alone document to justify medical necessity for each session. As part of your contract with the insurance company, they can request your record to review and audit.
If you accept insurance in your practice, it is very important to remember while documenting that the insurance company may read your therapy notes. You may not want to include intimate and personal details in the therapy notes, such as descriptions of a client’s fantasies or dreams.
Your therapy notes should include the information necessary to support and demonstrate medical necessity for treatment and the session conducted.
Some of the information that supports medical necessity for insurance companies includes:
- Billable diagnosis (you should enter the same diagnosis you entered on the insurance claim form)
- Observations of the client during the session that support the diagnosis
- What you did in the session that directly relates to this diagnosis
- Treatment goals and objectives (from the treatment plan) that you addressed in the session
- Any progress the client may have made toward treatment goals
- How the client responded to the treatment during the session
- Did the client show any improvement? Decline? Maintain stability?
How do therapy notes ensure greater continuity of care for your client?
Therapy notes tell a story of how your client progresses in treatment. When other service providers, physicians, or support review well-written therapy notes, they can better provide services and care for your client. If you incorporate observations, goals, interventions, and the client’s response to treatment, your therapy notes explain how your client progresses through treatment, what you did in the sessions, and how the client responded.
Other providers who may request your notes might include:
- Psychiatric providers
- Primary care doctors
- Agency case managers
- New therapists who treat your client after discharge
- Additional therapists involved in your client’s care such as a marriage counselor
- Inpatient treatment centers
How can therapy notes help a therapist track treatment progress?
Prior to starting a new session with your client, take a few minutes to read over the therapy notes from the previous session. This time can help to remind you of what occurred during the last session and what you planned for the current session. This practice can help you to follow through on what was addressed in the previous session, follow up on homework assigned to the client, and continue to monitor progress on the treatment.
When therapy notes from the previous session are fresh in your mind, you might be more likely to adhere to the goals and objectives addressed in the treatment plan in the current session. You may be better able to assess progress, or lack of progress, in treatment and better plan for today’s session.
Legal and ethical considerations in therapy notes telehealth
Your therapy notes do not fall under the protection of HIPAA. Therefore, other parties can request the therapy notes that you keep in your client record. If you bill an insurance company for the session, they can request to review your therapy notes at any time as part of their contract with you and with the client.
Other parties can request therapy notes with authorization. Some requestors may be outside the usual scope of practice. For example, if you have a client going through a legal case, the attorney, with a signed release from your client, can request the therapy notes from your sessions.
Other possibilities include:
- Disability insurance companies
- Treatment centers
- Vocational agencies
- Community agencies or non-profit organizations involved in your client’s care
Also, keep in mind that your therapy notes can be subpoenaed and included in a legal case. Consequently, opposing parties, a jury, a judge, witnesses, or anyone in a courtroom may hear what you have written in your therapy notes.
Start 30-day Free Trial and explore TheraPlatform. HIPAA Compliant Video and Practice Management Software for Therapists.
Ethical considerations when writing your therapy progress
Note care and consideration when writing your therapy notes. In addition to external requestors, your client can also request to have any part of their client record, including their therapy notes. For these reasons, you want to write notes that remain sensitive to your client, are accurate, and do not express any words of judgment.
Some steps to writing an ethically sound note and incorporating medical necessity are:
- Do not use words and phrases such as “it appears”, “it seems”, or “I think”
- Use words such as “demonstrates”, “presents with”, “client reports”, or “engaged in”
- Avoid absolute qualifiers such as “always” and “never”
- When quoting a client, make sure to use direct quotes around the communication
- Do not write about client financial arrangements with your practice, balances owed, or agreements to future payments
Most therapists do not enjoy writing therapy notes. However, if you can create a template based on the information addressed in this article, the process can be less stressful for you.
How EHR software can help with therapy notes for telehealth
Electronic health record (EHR) and practice management software, such as TheraPlatform, can make note taking for telehealth fast, flexible and accurate.
Benefits of using EHR for therapy notes for telehealth
Consistent notes with a library of note templates
Having an EHR with built-in note templates can help therapists write more accurate, high-quality, consistent and concise teletherapy notes. An EHR can also provide a central location to store and access notes helping therapists stay more organized.
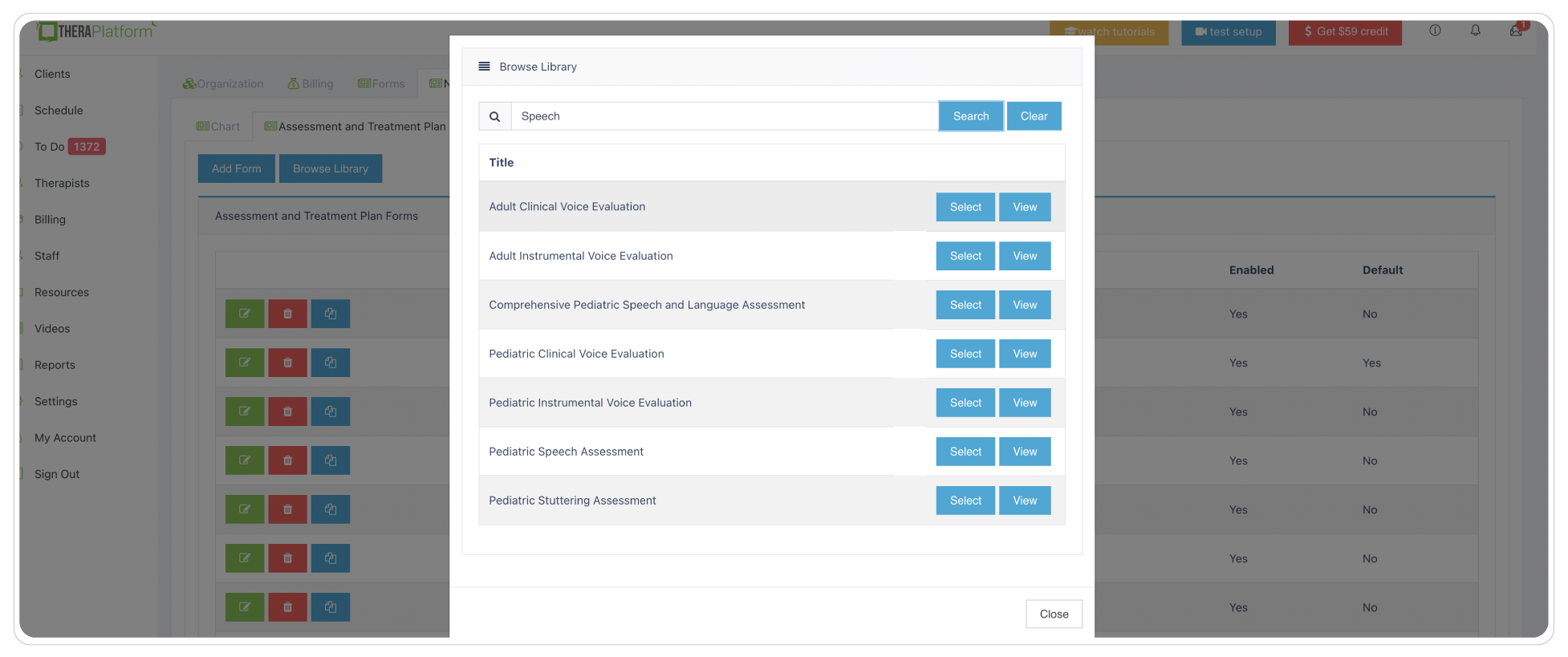
Flexible note template builder
Many therapists have their own preferences for documenting sessions. Some prefer SOAP note templates to help organize Subjective, Objective, Assessment and Plans. Other therapists prefer a single field that allows them to craft their own telehealth note form. Yet other therapists use checkboxes on their note templates for repetitive information such as techniques or mental status. Using a comprehensive, easy-to-use note template builder can help you save time and document your way.
HIPAA-compliant storage of telehealth notes
Creating and storing your telehealth notes in an encrypted, secure software program protects your clients’ data giving your peace of mind. In addition to bank-level security standards, TheraPlatform also provides private practice therapists with a signed, legally-binding Business Associate Agreement that helps protect PHI between HIPAA compliant entities.
Securely and easily share your telehealth therapy notes with clients
Clients may request telehealth therapy notes for their own records in an effort to understand their diagnosis or treatment or to build therapeutic rapport. Superbill clients are another group of clients who may request notes in case of an insurance audit. The ability to access and share your notes quickly and securely through an EHR saves time and frustration that normally accompanies paperwork requests.
TheraPlatform’s HIPAA-compliant EHR for therapists, allows you to securely share telehealth therapy notes with clients through the client portal.
Duplicate notes from previous sessions
SOAP note data might repeat with certain clients from session to session. In these cases, the ability to copy notes and pull information forward from one session to the next on TheraPlatform can be a huge time saver. Most importantly, these re-recorded notes can be edited for recency and relevance to eliminate inaccuracies and avoid over-duplication in client records.
Client signatures in a snap
TheraPlatform's Pro and Pro Plus plans offer documentation features with the ability to request signatures from clients on notes. Your client can download and print this document. This is important in telehealth where it’s suggested that providers confirm the identity, location and location safety for telehealth sessions.
Efax your notes from your clients’ chart with a click of a button
Eliminate maneuvering between two services with an integrated solution like TheraPlatform with efax integration. This add-on integration saves time and lowers costs as incoming and outgoing documents like SOAP notes, and other documents are sent via fax right from TheraPlatform. You can also file received faxes with a click of a button under the client’s charts.
Using an all-in-one EHR, practice management and teletherapy tool like TheraPlatform can further help reduce the stress involved in writing therapy notes. TheraPlatform offers a free, 30-day trial with no credit card required. Cancel anytime.
Sources
Huggins, R. “Telemental Health Documentation: 5 Things to Write Down.” Person Centered Tech. August 22, 2018. Accessed March 12, 2023.
US Department of Health and Human Services. “HIPAA Privacy Rule and Sharing Information Related to Mental Health.” Accessed March 13, 2023.
More resources
- Wiley treatment planners
- Therapy notes blog
- Therapy resources and worksheets
- Therapy private practice courses
- Ultimate teletherapy ebook
- The Ultimate Insurance Billing Guide for Therapists
- The Ultimate Guide to Starting a Private Therapy Practice
Free video classes
- Free mini video lessons to enhance your private practice
- 9 Admin tasks to automate in your private practice